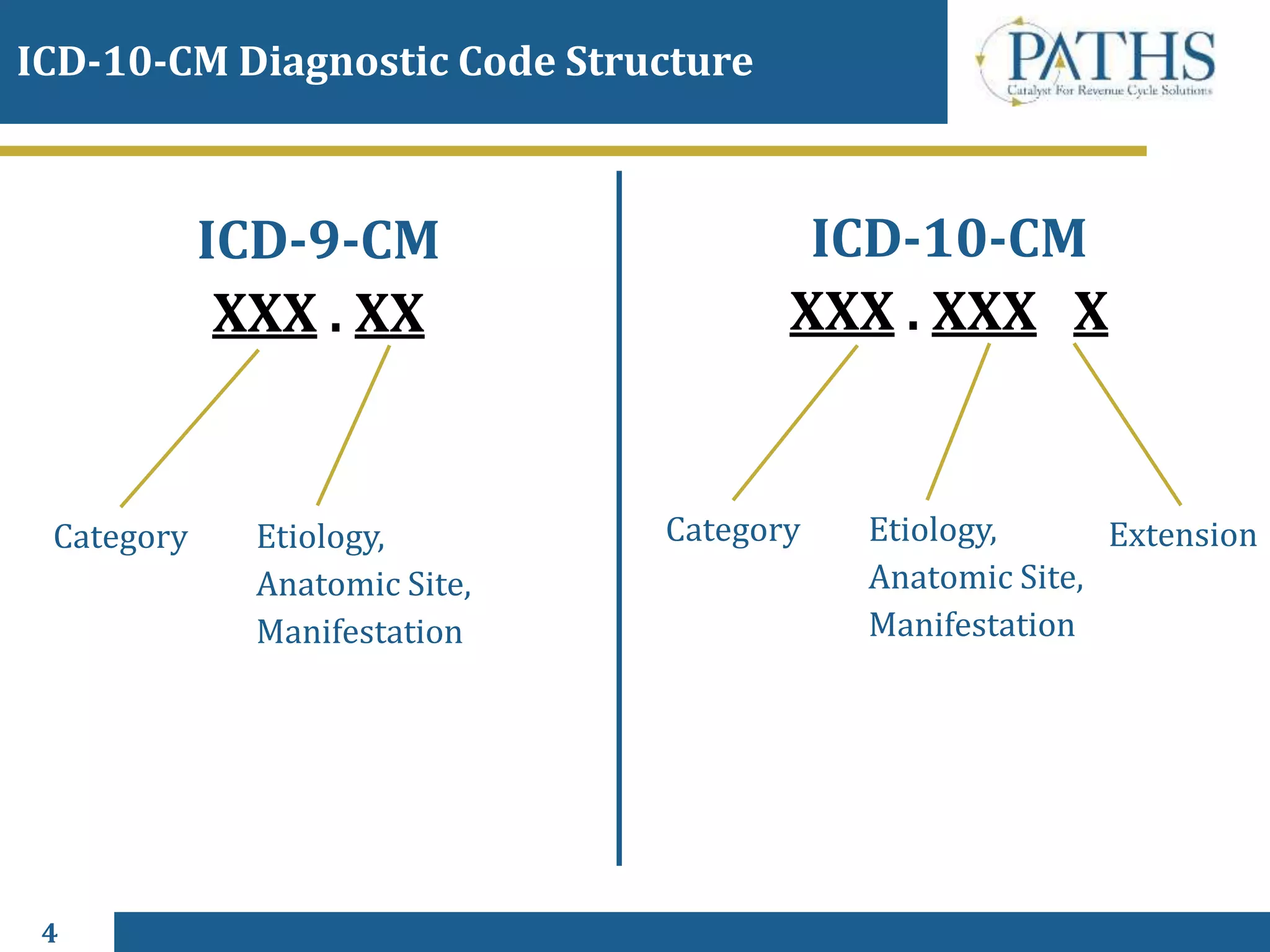
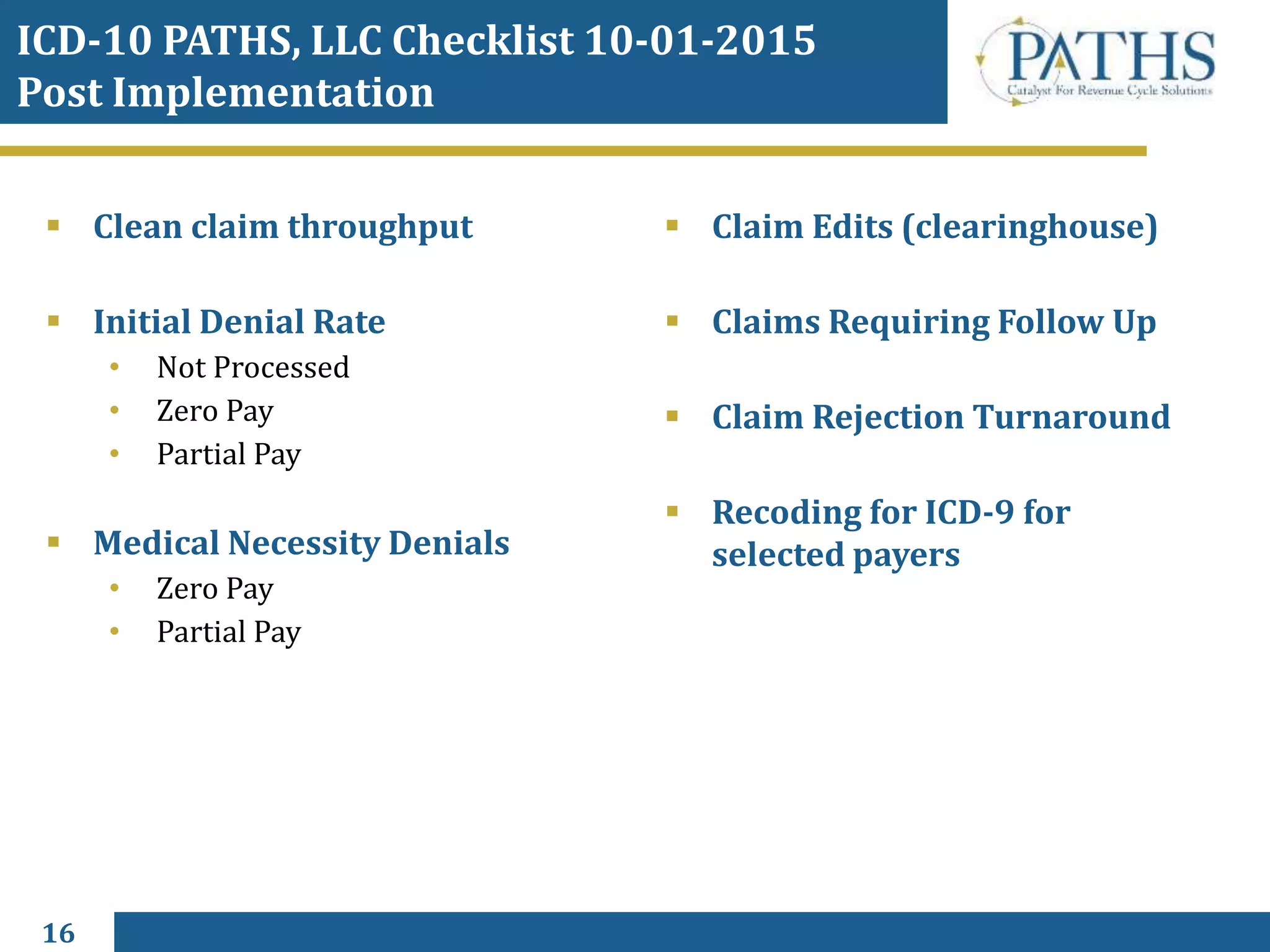
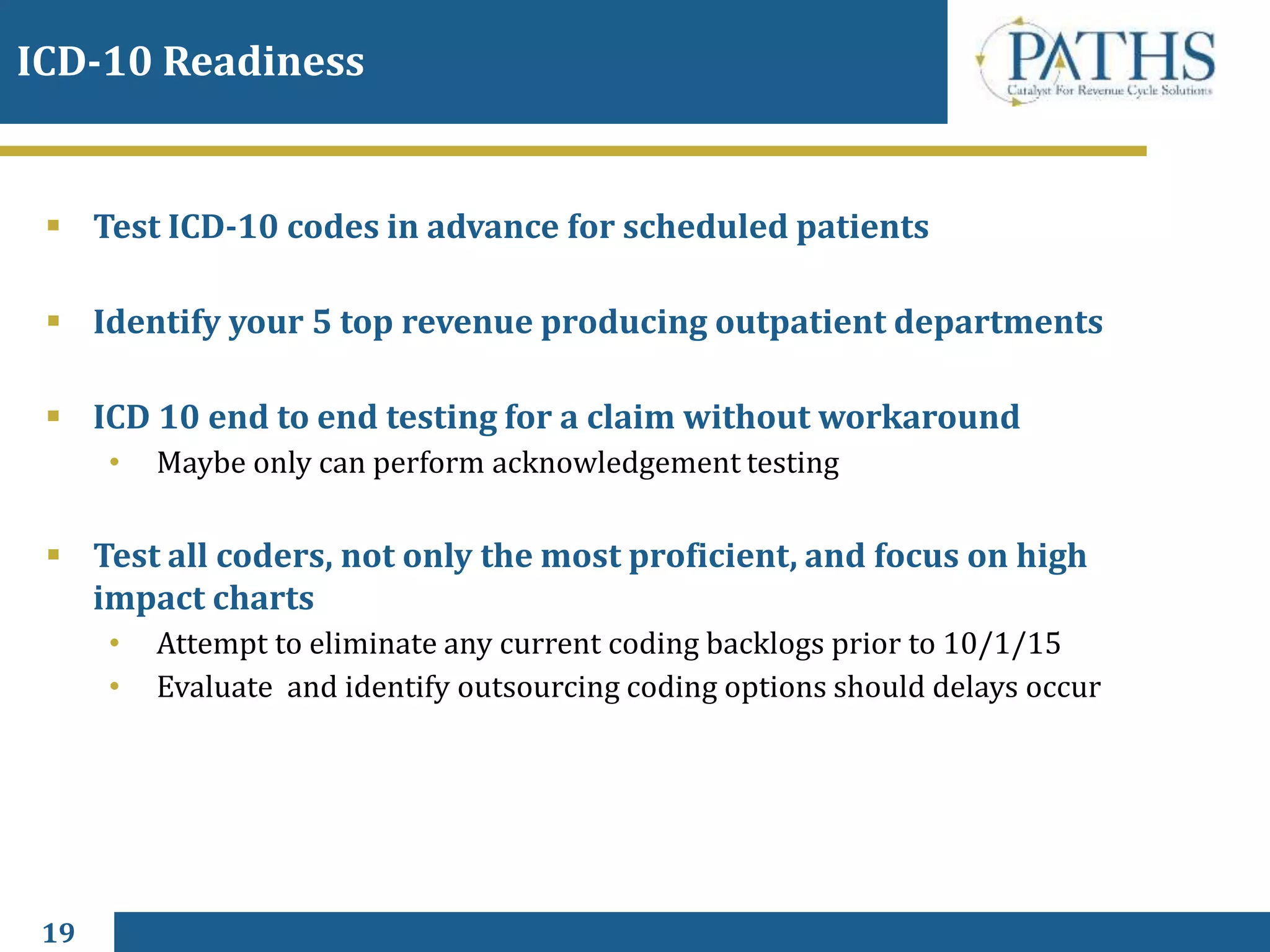
The document provides an overview of ICD-10, including definitions of ICD-10-CM and ICD-10-PCS, key differences from ICD-9, code structure changes, the October 1, 2015 implementation date, resources available, potential impacts of implementation, stakeholders involved, and considerations for revenue cycle management and readiness.