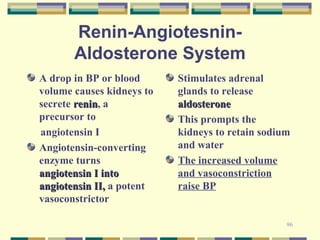
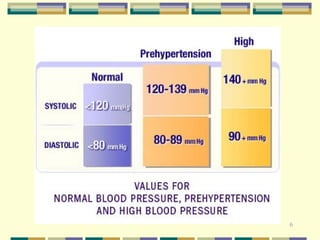
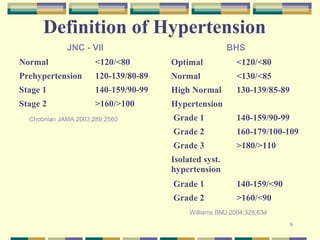
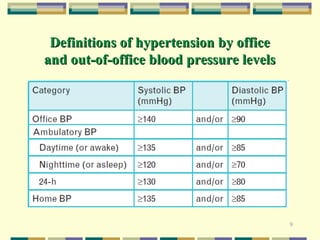
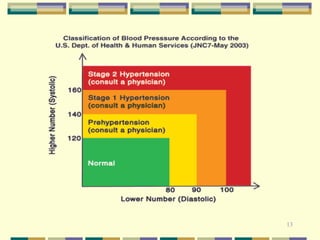
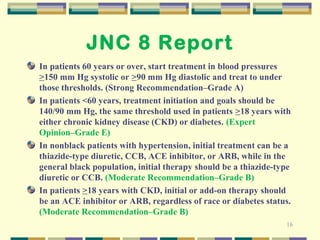
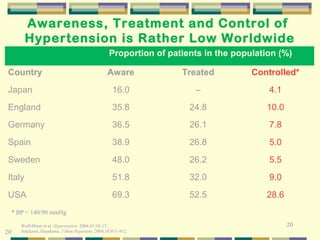
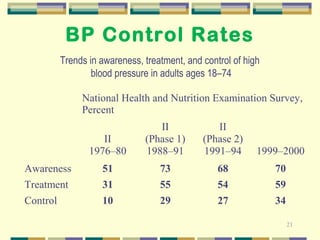
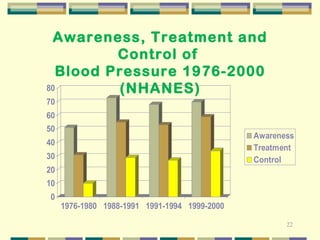
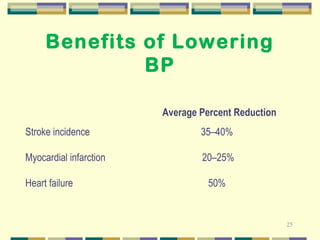
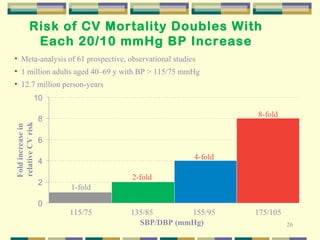
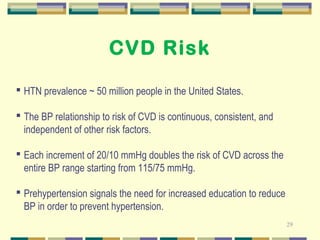
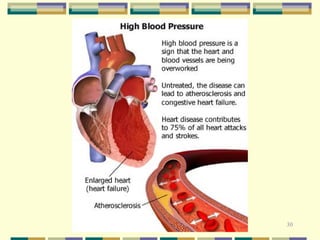
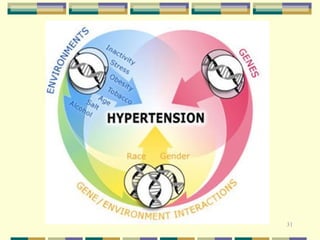
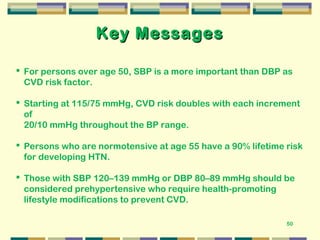
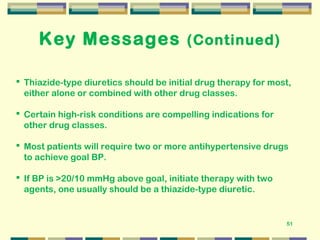
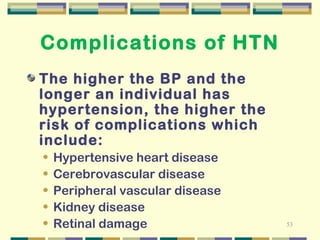
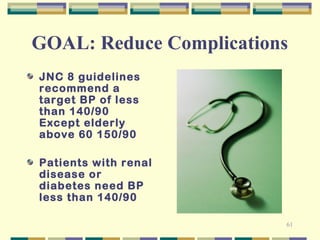
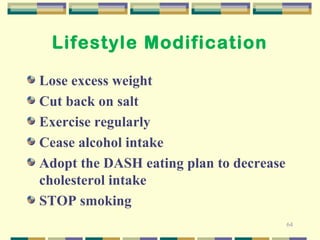
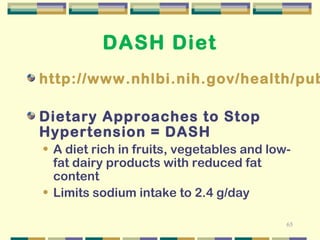
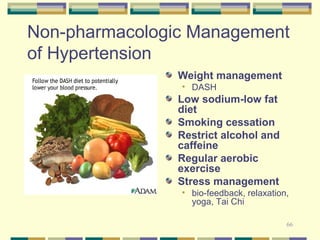
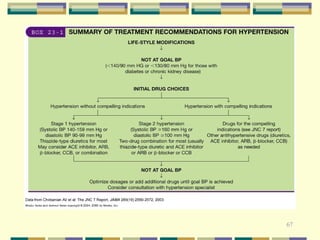
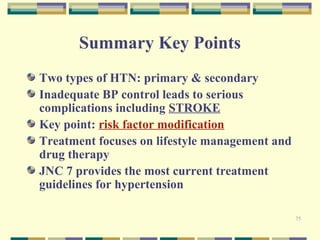
Hypertension is a major public health problem that significantly increases the risk of heart disease, stroke, and kidney disease. While medications can effectively treat hypertension, lifestyle modifications like following the DASH diet, reducing sodium intake, regular exercise, weight management, and limiting alcohol and tobacco use are important first steps to help prevent and control high blood pressure. The guidelines recommend treating hypertension with medications if lifestyle changes do not lower blood pressure enough, with a goal of reducing blood pressure to under 140/90 mmHg to minimize complications.



![90
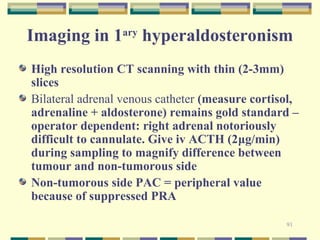
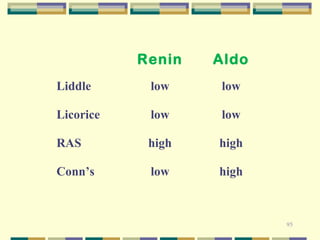
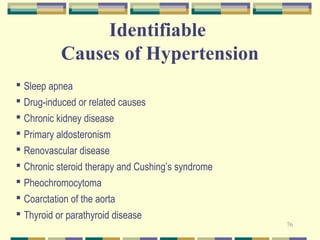
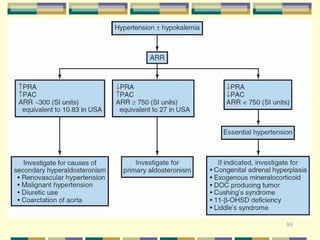
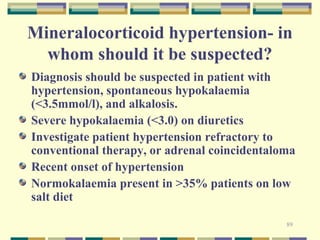
Clinical features of
hyperaldosteronism
Mild to severe hypertension
Sodium retention + intravascular vol exp
®mineralocorticoid escape
Resetting of osmostat (thirst provoked at higher [Na+])
K+ loss (kaliuresis) +/- low serum K+ (unprovoked: rule out
diuretics, laxatives, vomiting, herbal supplements)
Suppression of renin generation (rule out drugs,excessive
dietary sodium intake)
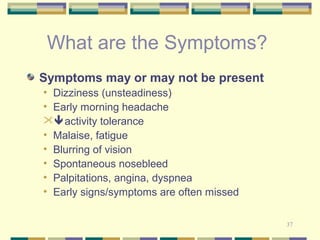
Polyuria, nocturia,fatigue,cramps, Mg++↓
Exclude liquorice abuse / carbenoxolone therapy
NB minor mineralocorticoids DOC, compound B](https://image.slidesharecdn.com/htn-2014-140916012549-phpapp01/85/Hypertension-2014-update-90-320.jpg)