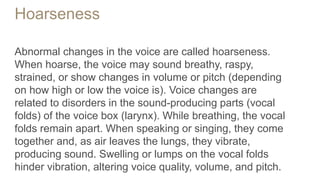
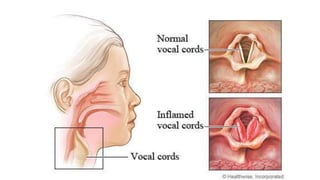
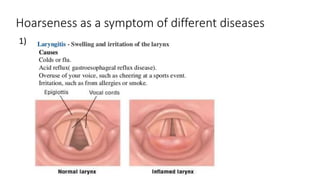
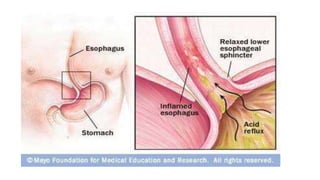
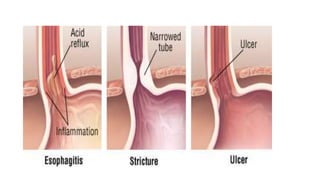
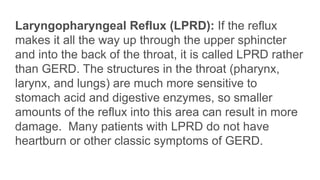
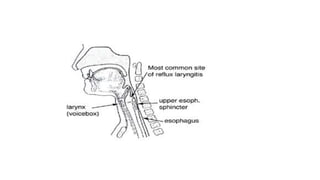
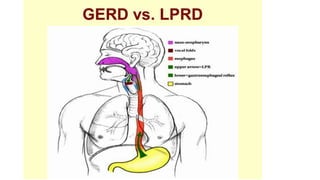
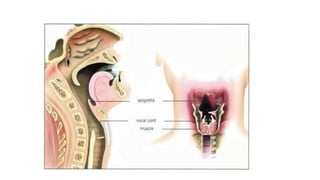
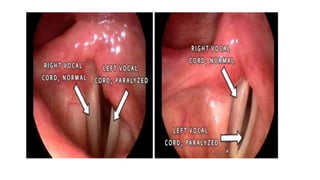
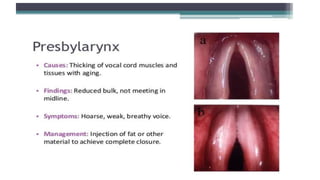
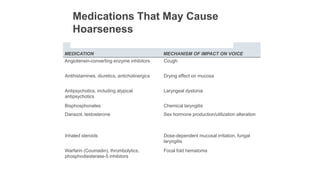
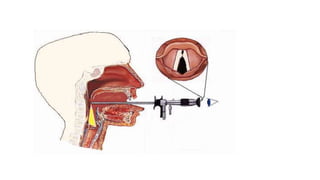
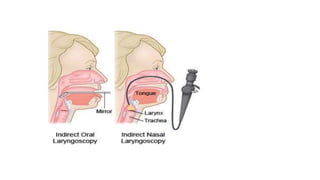
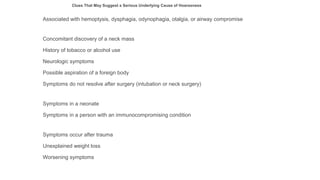
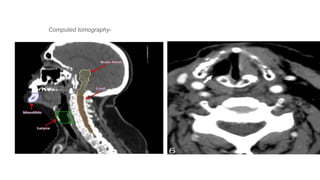
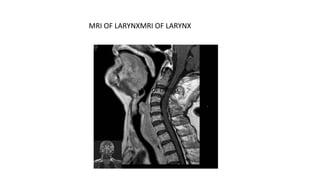
Hoarseness is an abnormal change in the voice that can be caused by disorders of the vocal folds. Symptoms include a breathy, raspy, strained or abnormal pitch or volume. Common causes discussed include benign vocal fold lesions from overuse, vocal fold hemorrhage from yelling, gastroesophageal reflux, laryngopharyngeal reflux, smoking, and neurological disorders. Evaluation includes laryngoscopy and other imaging tests if needed. Treatment depends on the underlying cause but may include voice therapy, antireflux therapy, corticosteroids, antimicrobials, botulinum toxin injections, or surgery. Preventive measures like hydration and avoiding irritants can help lower risk of hoarseness.