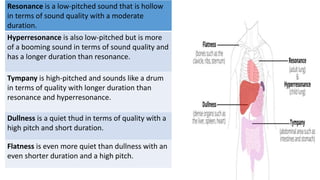
The document provides a comprehensive overview of health history taking and physical examination techniques in nursing. It details the importance of effective communication, systematic interview phases, and methods for collecting subjective and objective health data. Additionally, it outlines the principles of physical examination, including inspection, palpation, percussion, and auscultation, emphasizing the need for a patient-centered approach.