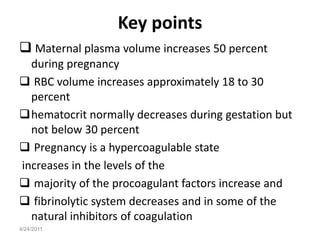
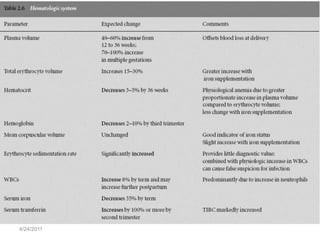
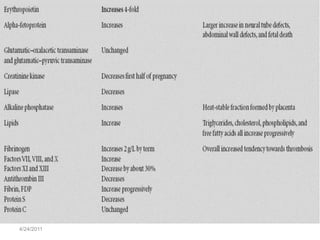
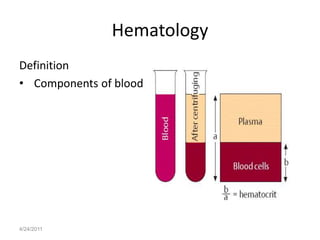
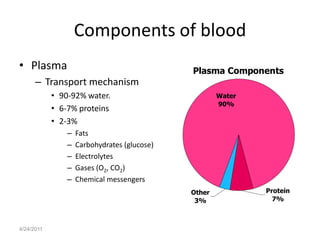
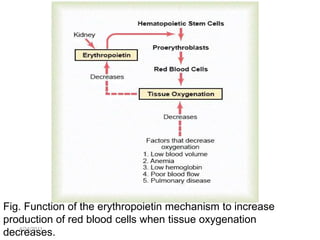
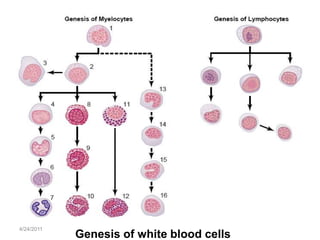
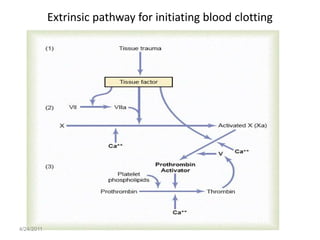
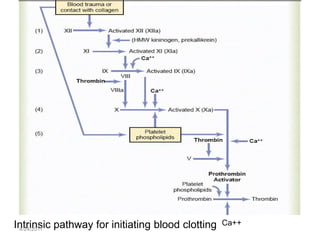
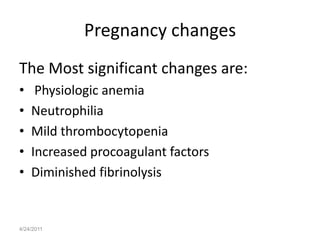
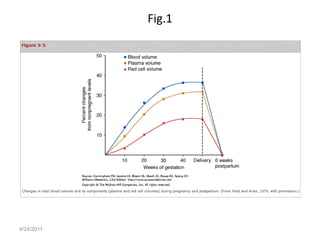
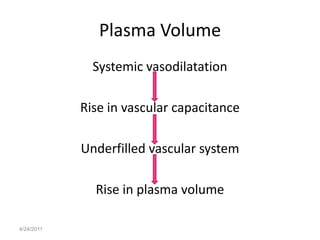
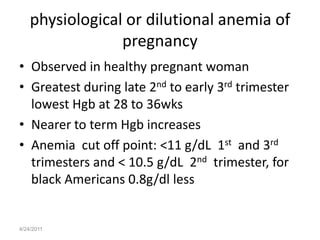
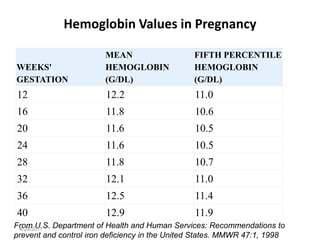
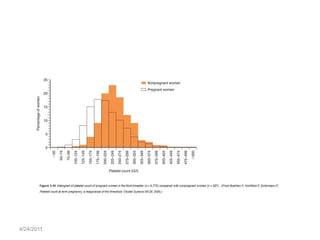
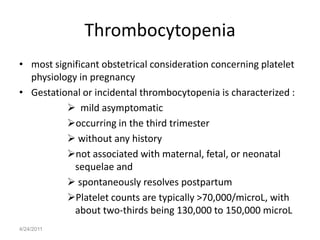
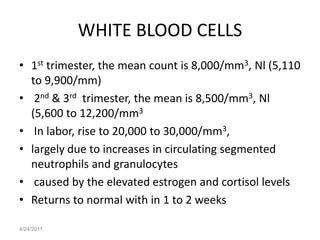
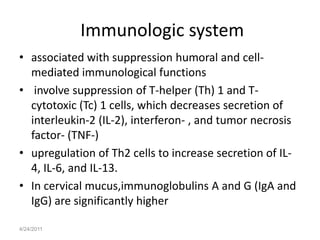
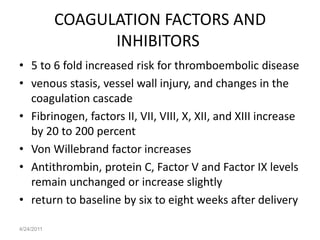
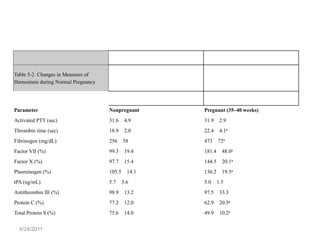
Hematologic changes occur during pregnancy including an increase in plasma volume by 10-15% and red blood cell volume by 20-30%. This causes a physiologic anemia. Platelet counts slightly decrease while white blood cell counts increase. Coagulation factors are elevated up to 200% making pregnancy a hypercoagulable state and increasing risk for thromboembolism. These changes support the increased metabolic demands of the growing fetus and placenta and help prevent blood loss during delivery.
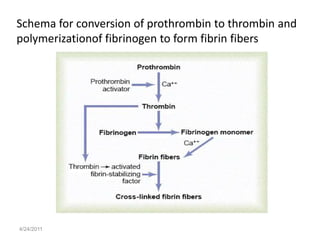
![Figure 3-11 The normal components of the coagulation cascade. (From Johnson RL:
4/24/2011
Thromboembolic disease complicating pregnancy. In Foley MR, Strong TH [eds]:](https://image.slidesharecdn.com/hematologicchangesofpregnancy-110424030452-phpapp02/85/Hematologic-changes-of-pregnancy-36-320.jpg)