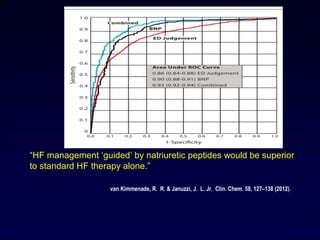
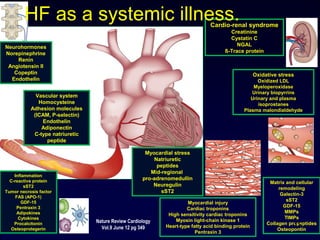
1) Heart failure is a major and growing public health problem, affecting over 15 million people in Europe with a prevalence of over 2-3% overall and 10-20% in those over 70 years old.
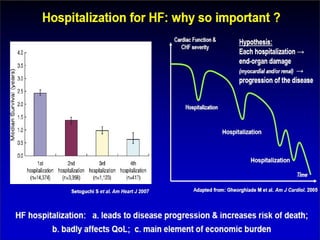
2) It is a primary cause of hospital admissions and readmissions, accounting for 5% of admissions and 40% of patients being readmitted or dying within a year. It represents a significant cost burden on healthcare systems.
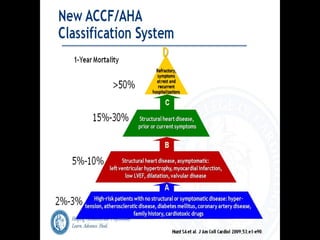
3) Diagnosis involves clinical examination, ECG, chest x-ray, echocardiography and natriuretic peptide levels of BNP or NT-proBNP which can help differentiate between possible and likely heart failure.
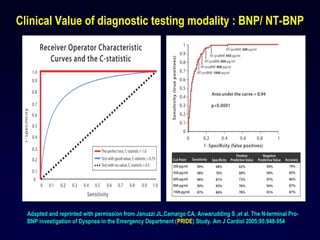
4) Heart failure is now recognized as a
![Heart failure -- Epidemiology
Prevalence • > 2% - 3% overall; 10% - 20% at > 70 yrs
• European society of cardiology countries : > 15
milion patients with heart failure and increasing
Burden • Primary cause of 5% of hospital admissions
• Present in 10% of hospitalized patients
• 2% of national health expenditure [60% - 70% of cost
due to heart failure hospitalization]
• 40% of patients admitted to hospital with heart
failure are dead or readmitted within 1 yr
Mcmurray J J Et Al Eur Heart J 2013; 33 [14]: 1787-1847
Dickstein K Et Al Eur Heart J 2006; 29: 2388-2442
FinalPathwaysDisease](https://image.slidesharecdn.com/heartfailureapi2014-160204104127/85/Heart-failure-api-2-320.jpg)
![Linking Short- term intervention with long-term benefit:
What is needed?
Better understanding of Acute Heart Failure pathophysiology
MORTALITY
• Myocardial injury [Tn
release]
• Renal dysfunction [CRS]
• Liver dysfunction
PREVENTION OF END-
ORGAN DAMAGE
Congestion
Viable but
dysfunctional
myocardium
Neurohormonal
& inflammatory
activation
Mechanisms which
can be targeted
Metabolic
factors
Hemodynamic
deterioration
[↑LVFP,↓ CO, ↓ PERFUSION]
Vascular resistance
/stiffness ↑
ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012 Reviewed by Ponikowski](https://image.slidesharecdn.com/heartfailureapi2014-160204104127/85/Heart-failure-api-9-320.jpg)


![Cumulative benefits of medical therapy on mortality. Adapted, with permission, from Fonarow GC, et al.
Potential impact of optimal implementation of evidence-based heart failure therapies on mortality. Am
Heart J 2011;161:1024-30.
Heart Failure Therapies
Beta-blocker
Beta-blocker +
ACEI/ARB
Beta-blocker +
ACEI/ARB+ ICD
Beta-blocker +
ACEI/ARB+ ICD+
HF education
Beta-blocker +
ACEI/ARB+ ICD+
HF education+
anticoagulation for
AF
Beta-blocker +
ACEI/ARB+ ICD+
HF education+
anticoagulation
for AF +CRT
ChangeinOddsof24-MonthMortality(%)
-39%
[-28% to -49%]
P < 0.0001
-63%
[-54% to -71%]
P < 0.0001 -76%
[-68% to -81%]
P < 0.0001
-81%
[-75% to -86%]
P < 0.0001
-83%
[-77% to -88%]
P < 0.0001
-81%
[-72% to -87%]
P < 0.0001](https://image.slidesharecdn.com/heartfailureapi2014-160204104127/85/Heart-failure-api-24-320.jpg)
![Number needed to treat for mortality
25
Guideline
recommended
therapy
Relative risk
reduction in
mortality
Number needed
to treat for
mortality
Number
needed to treat
for mortality
[ standardized
to 36 mths]
Relative risk
reduction in HF
hospitalisations
ACEI / ARB 17% 22 over 42 mths 26 31%
Beta blocker 34% 28 over 12 mths 9 41%
Aldosterone
antagonist
30% 9 over 24 months 6 35%
Hydralazine /
nitrate
43% 25 over 10 mths 7 33%
CRT 36% 12 over 24 mths 8 52%
ICD 23% 14 over 60 mths 23 NA
Reproduced with permission from Fonarow GC et al Am Heart j 2011; 161: 1024-30](https://image.slidesharecdn.com/heartfailureapi2014-160204104127/85/Heart-failure-api-25-320.jpg)