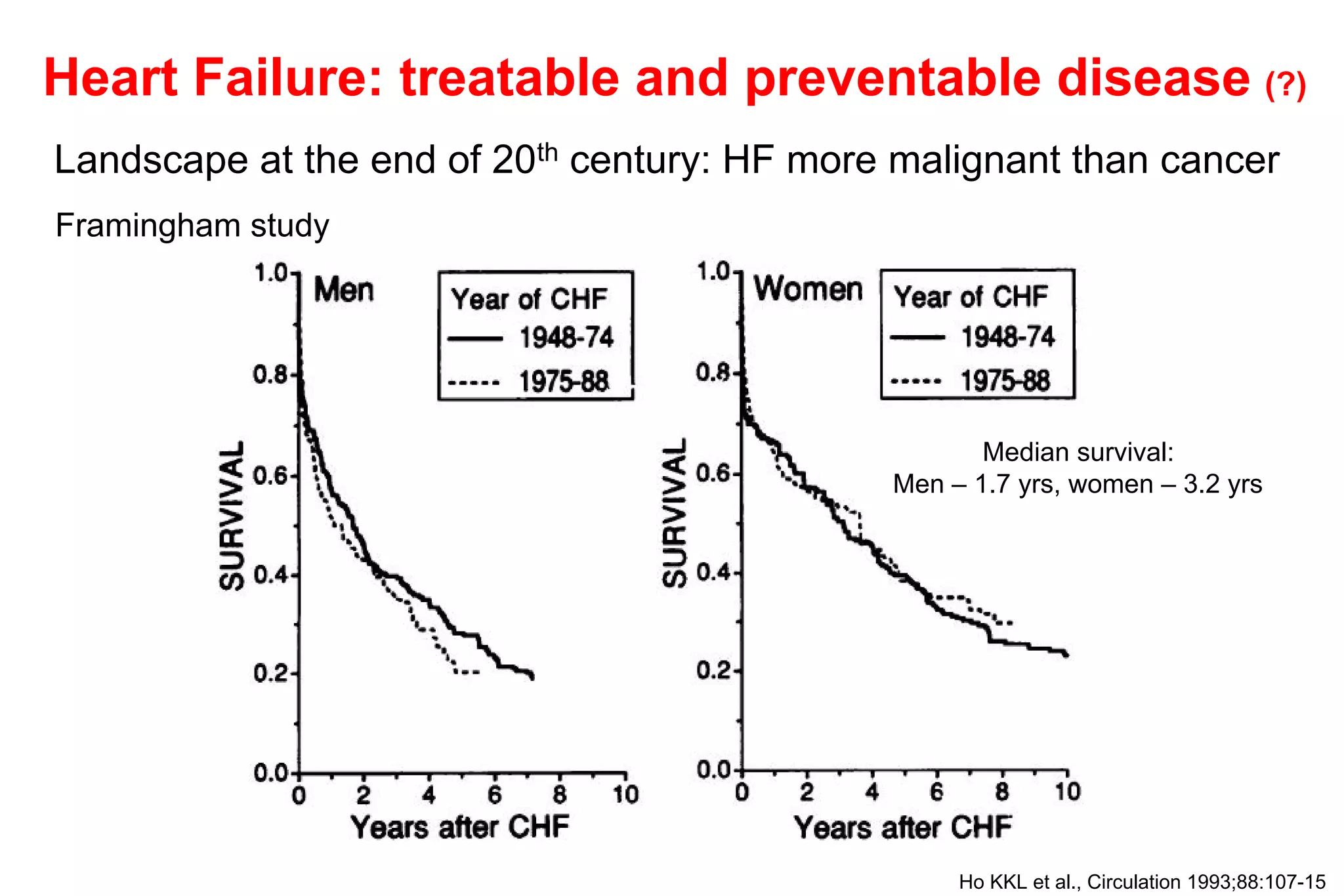
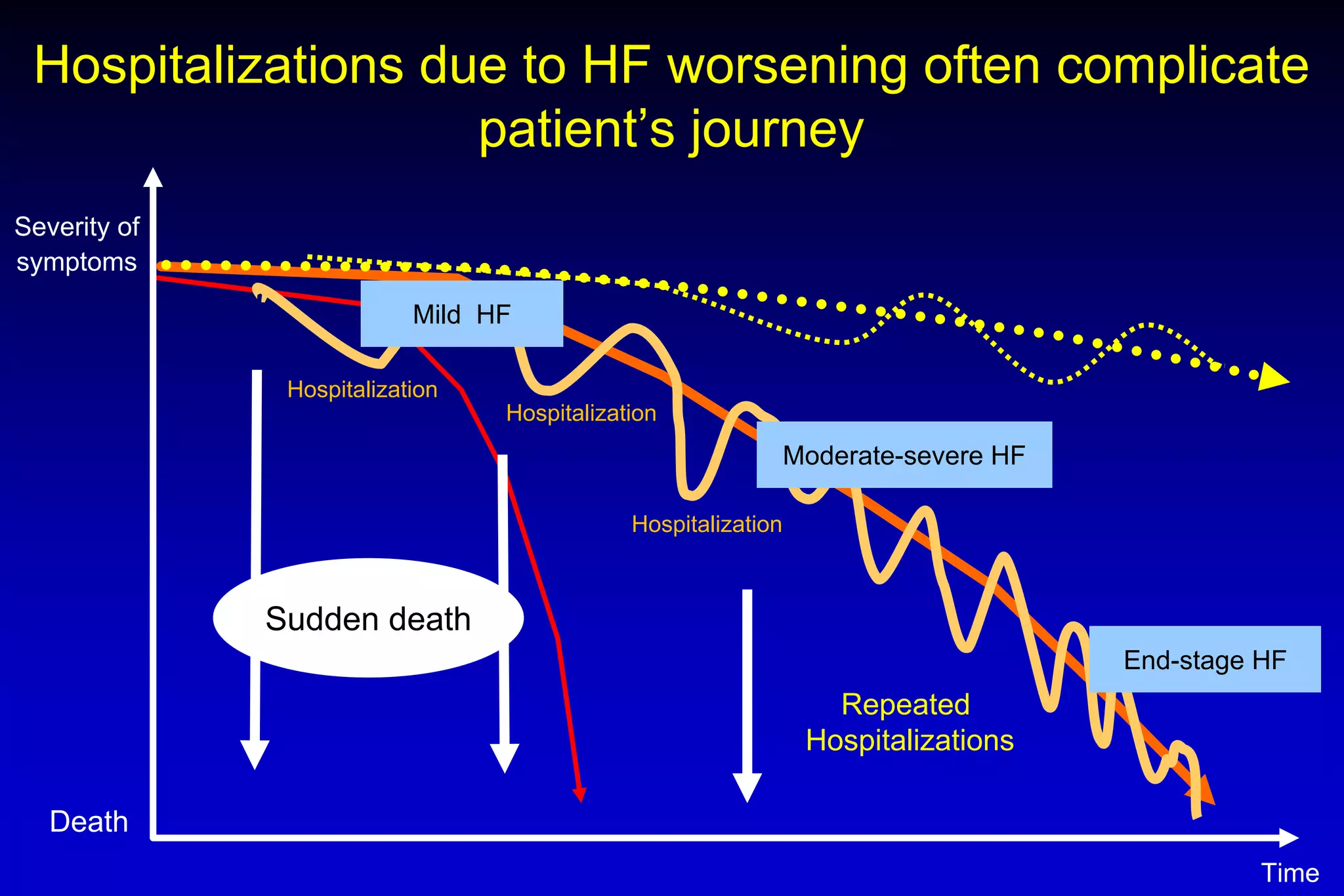
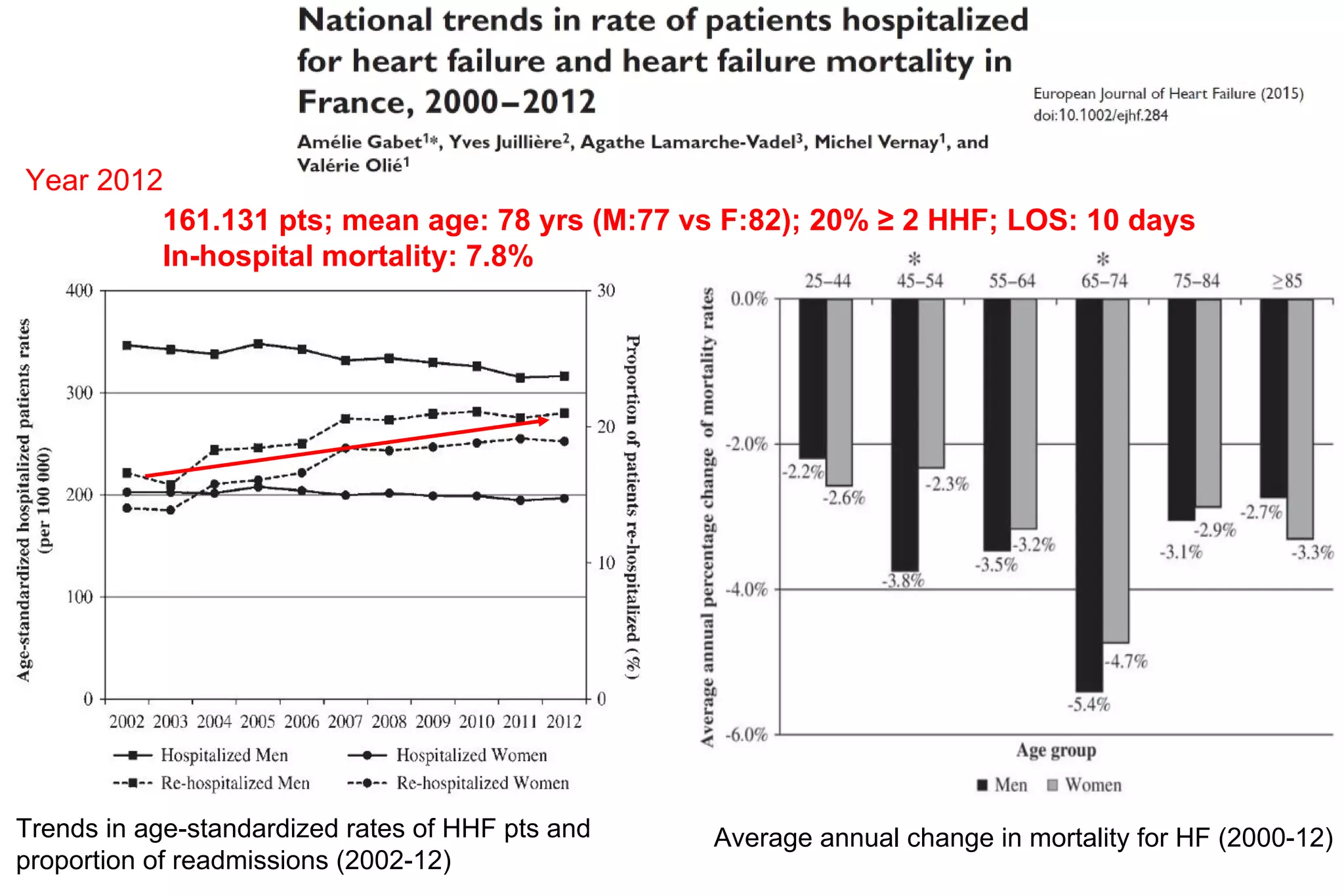
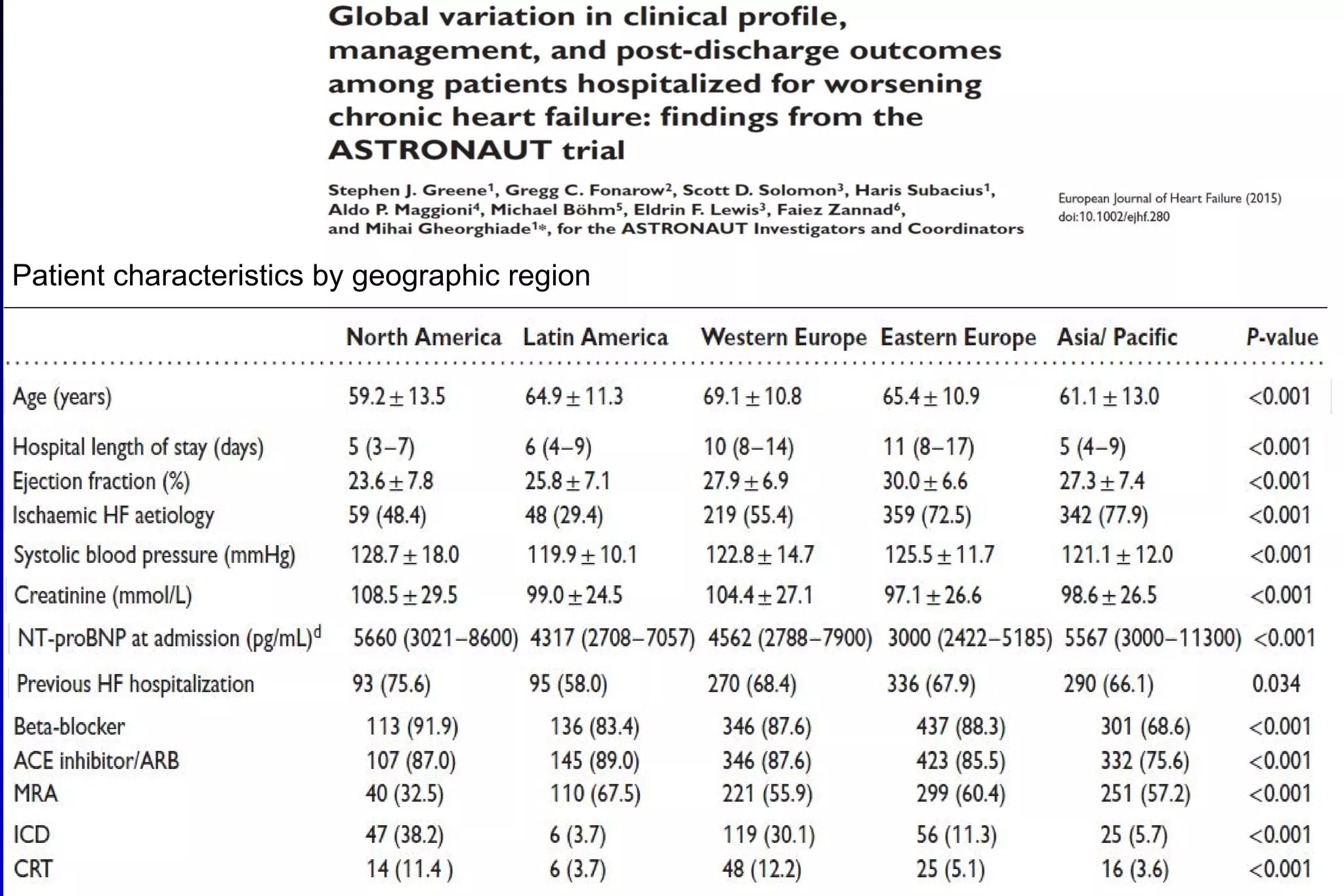
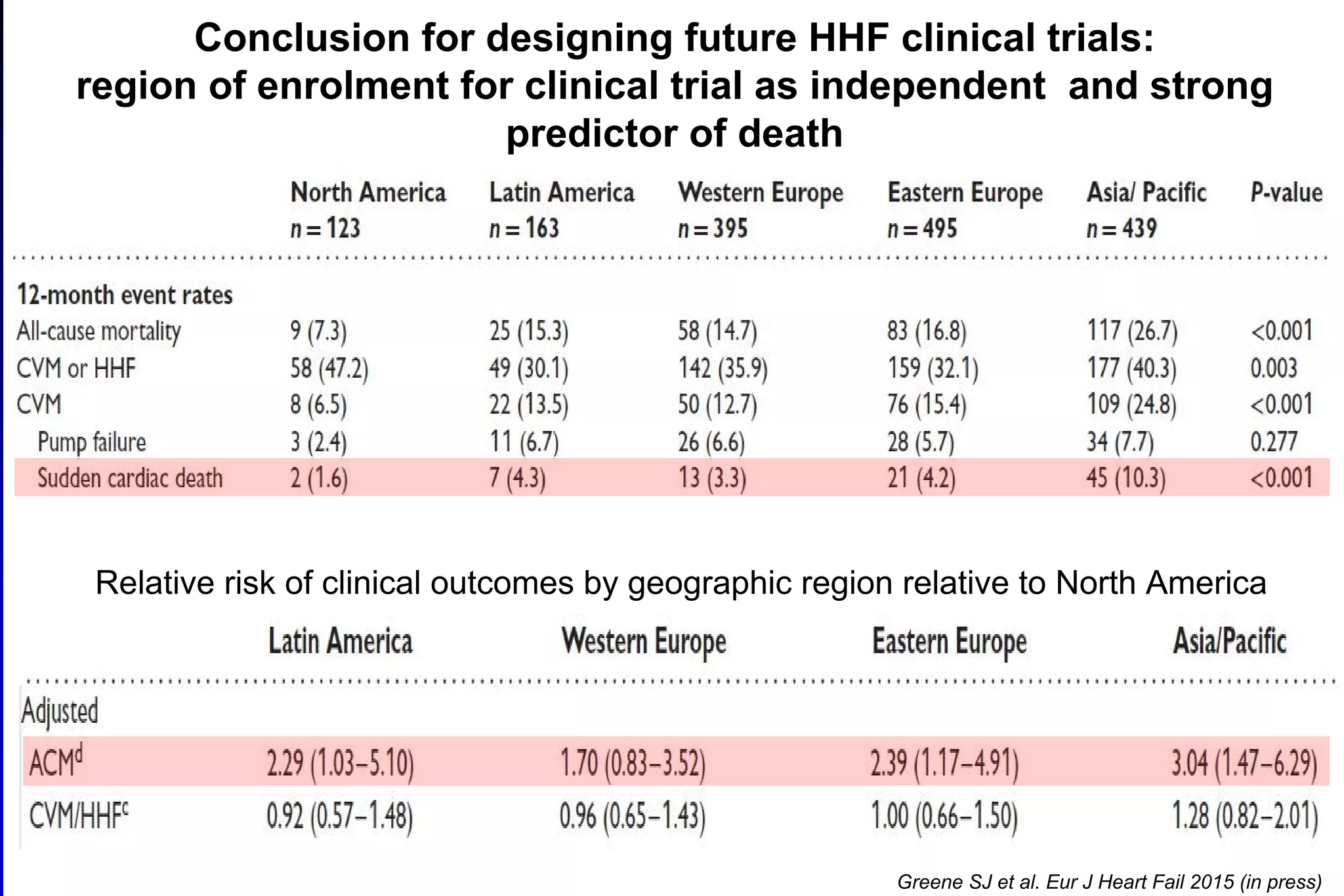
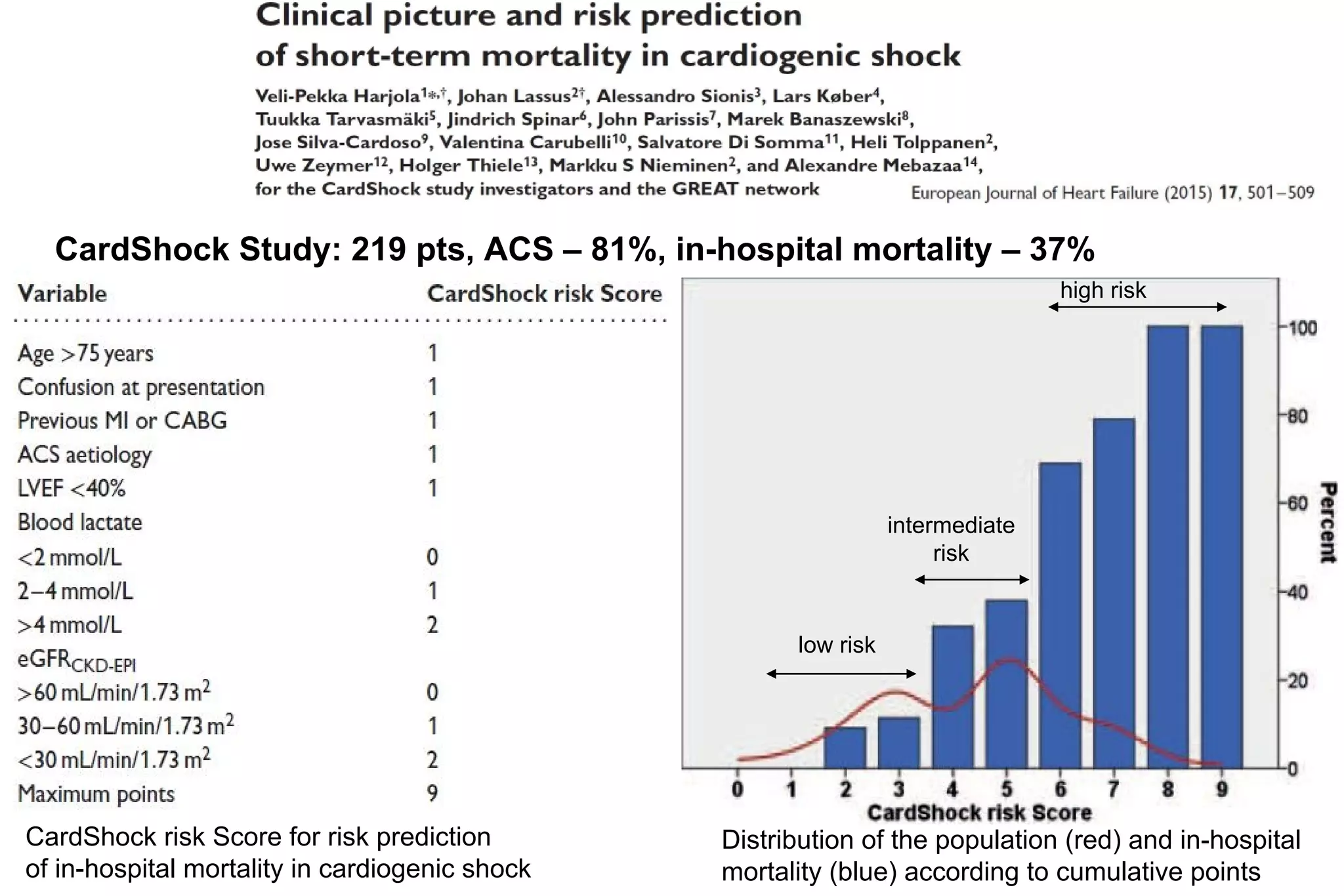
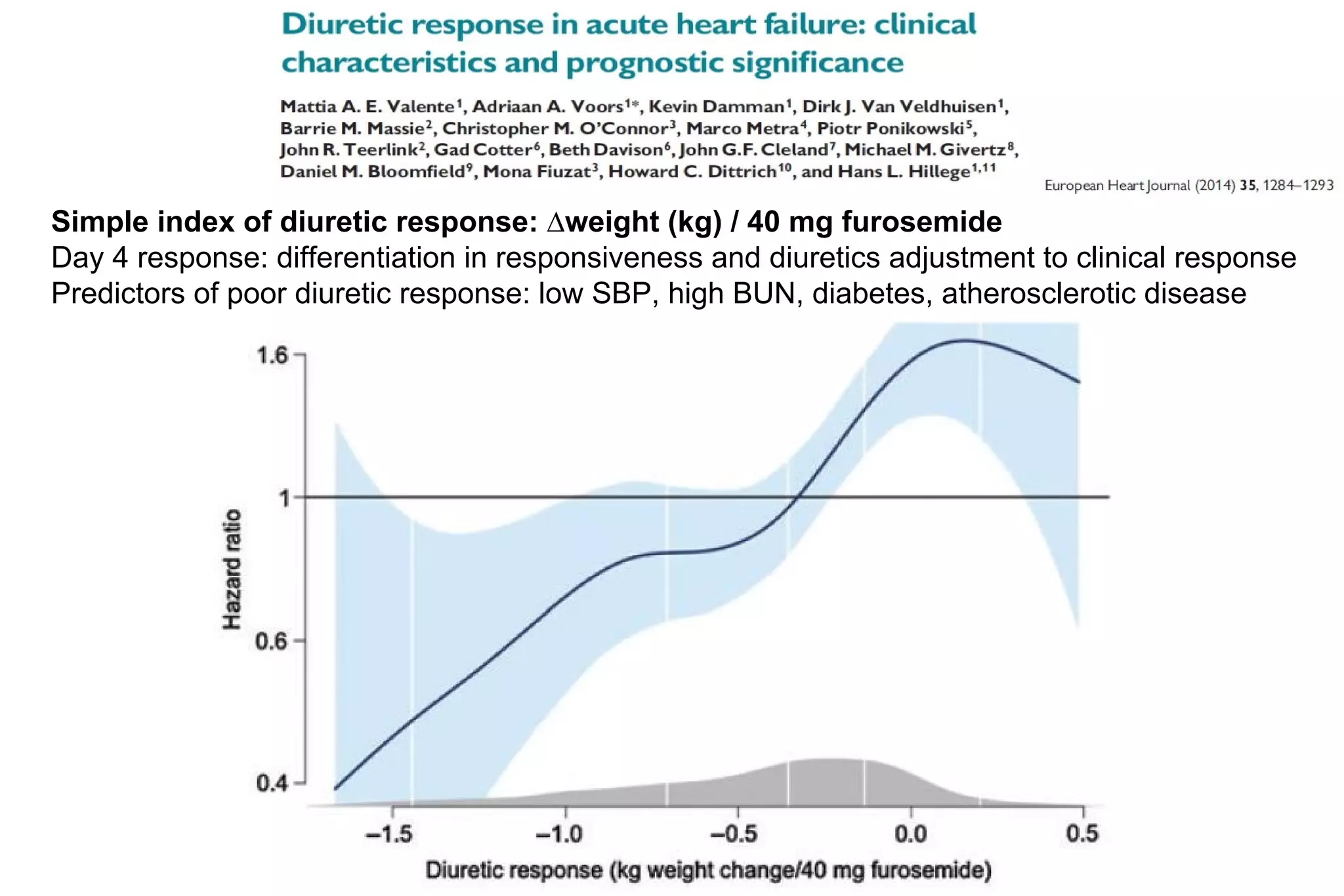
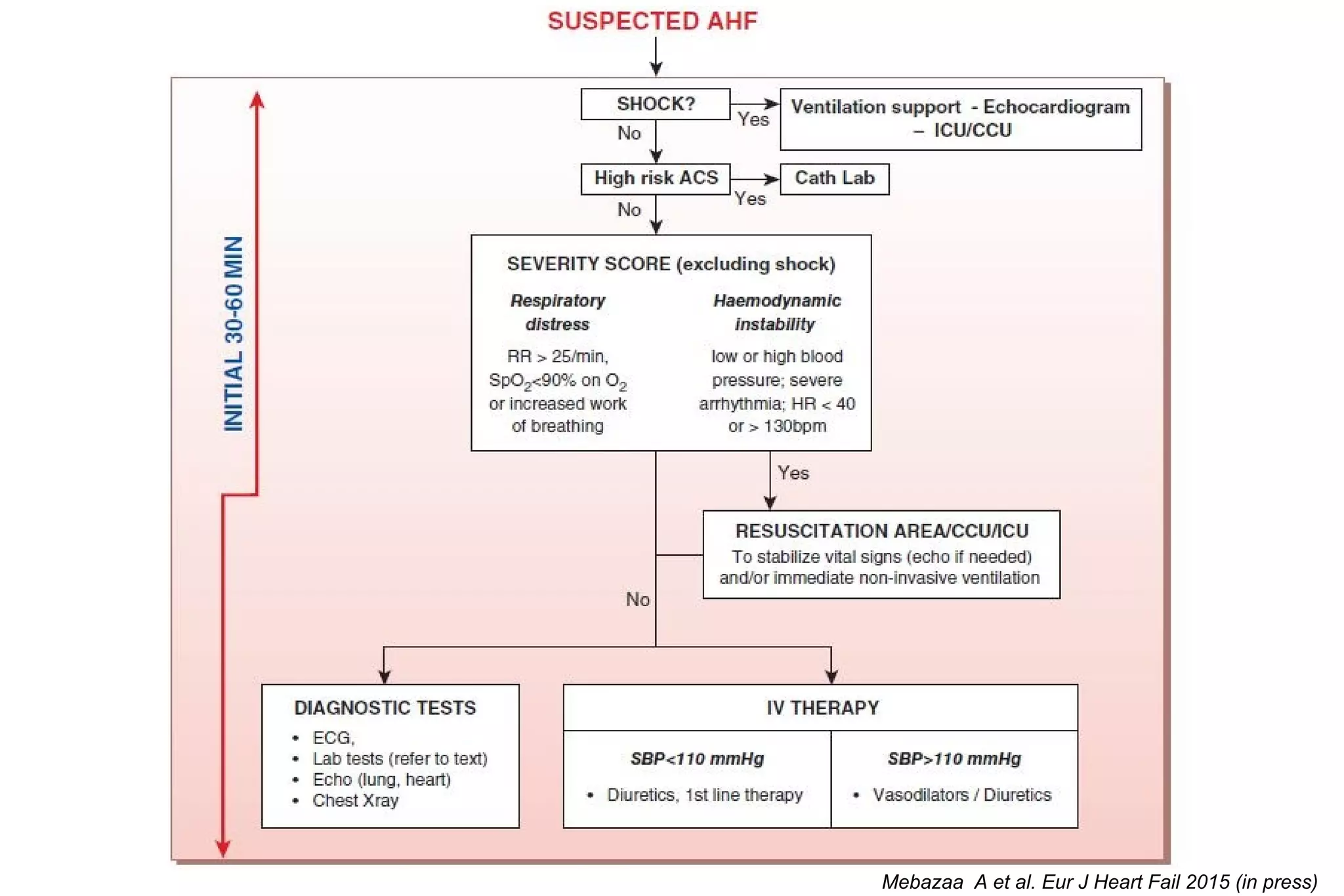
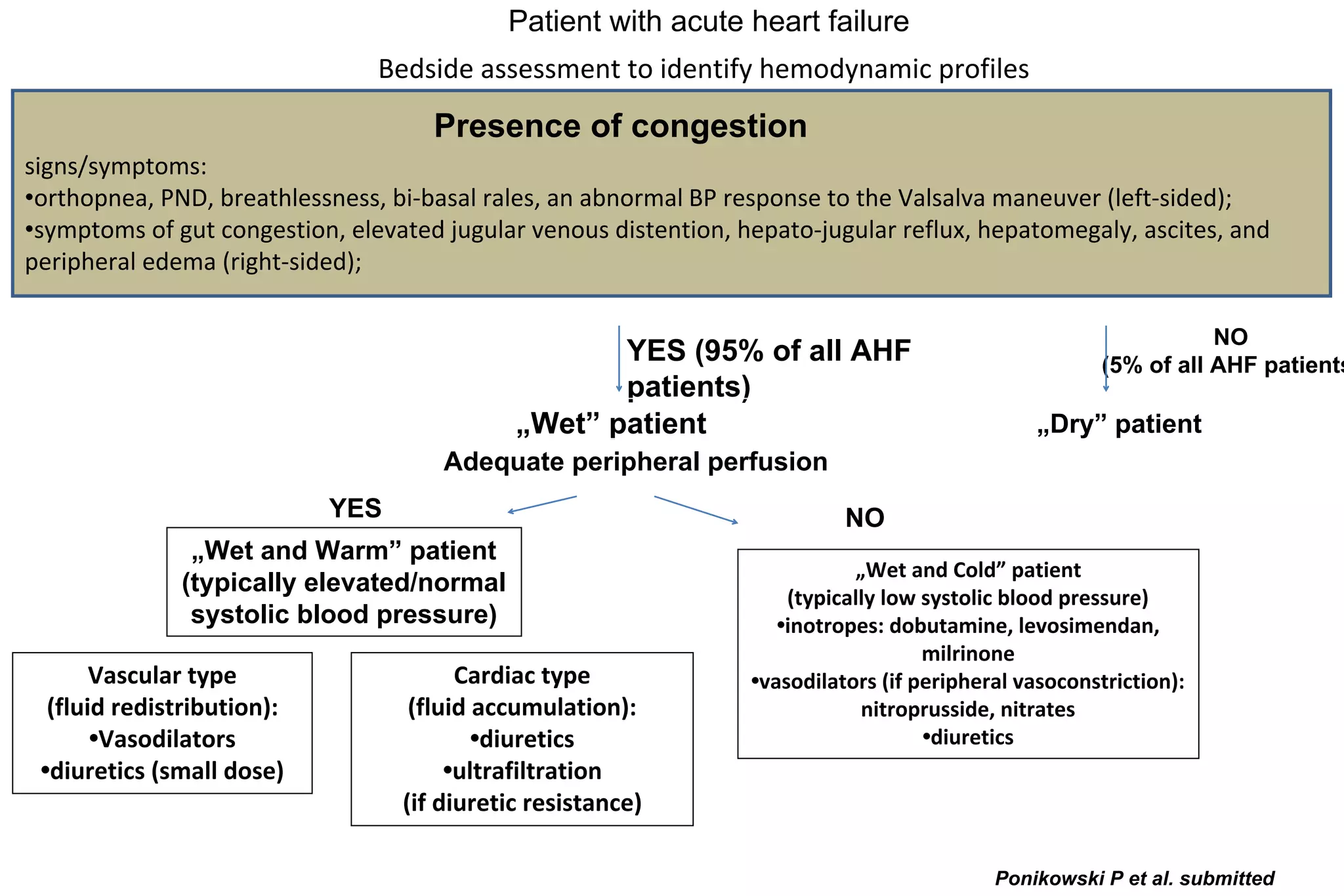
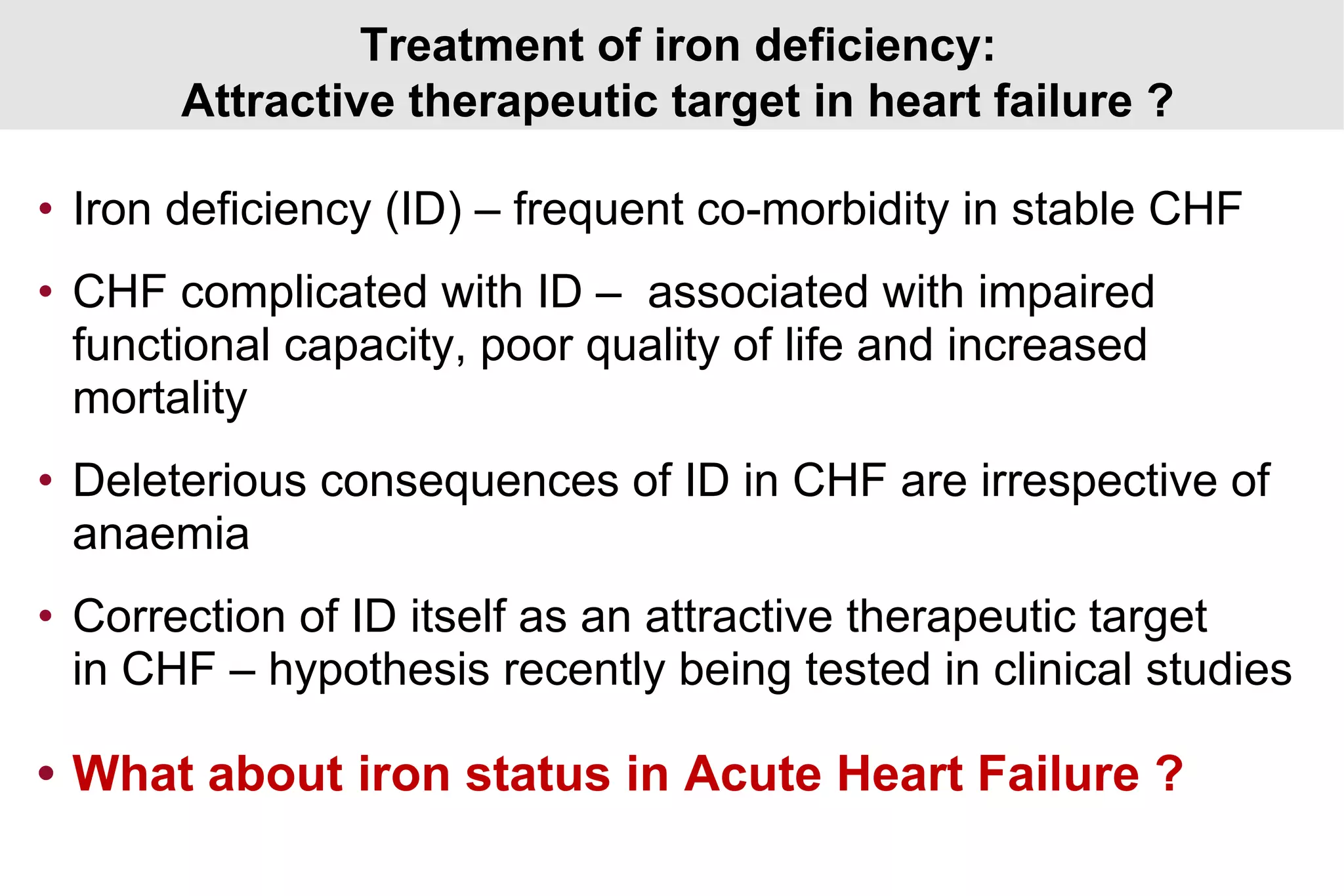
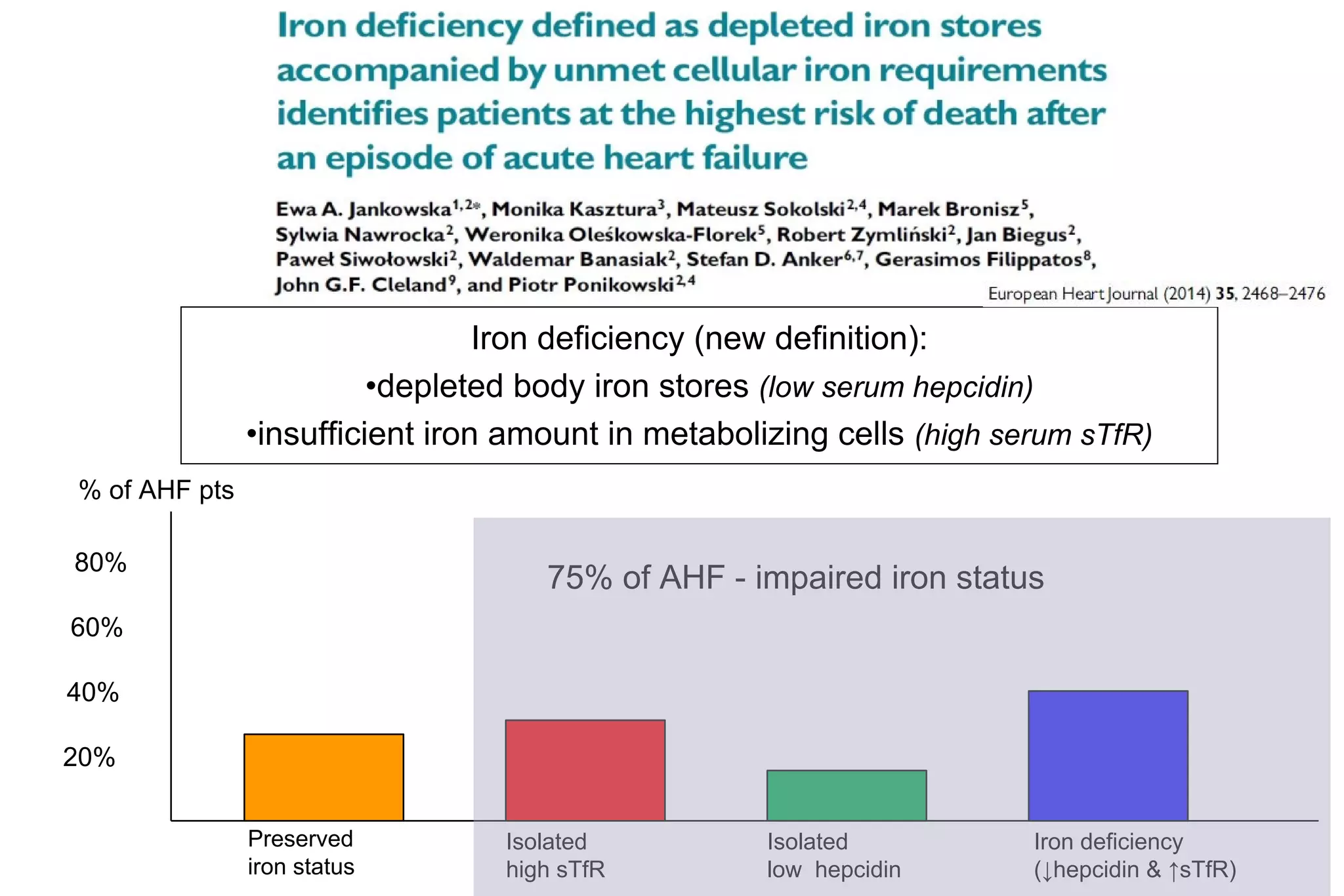
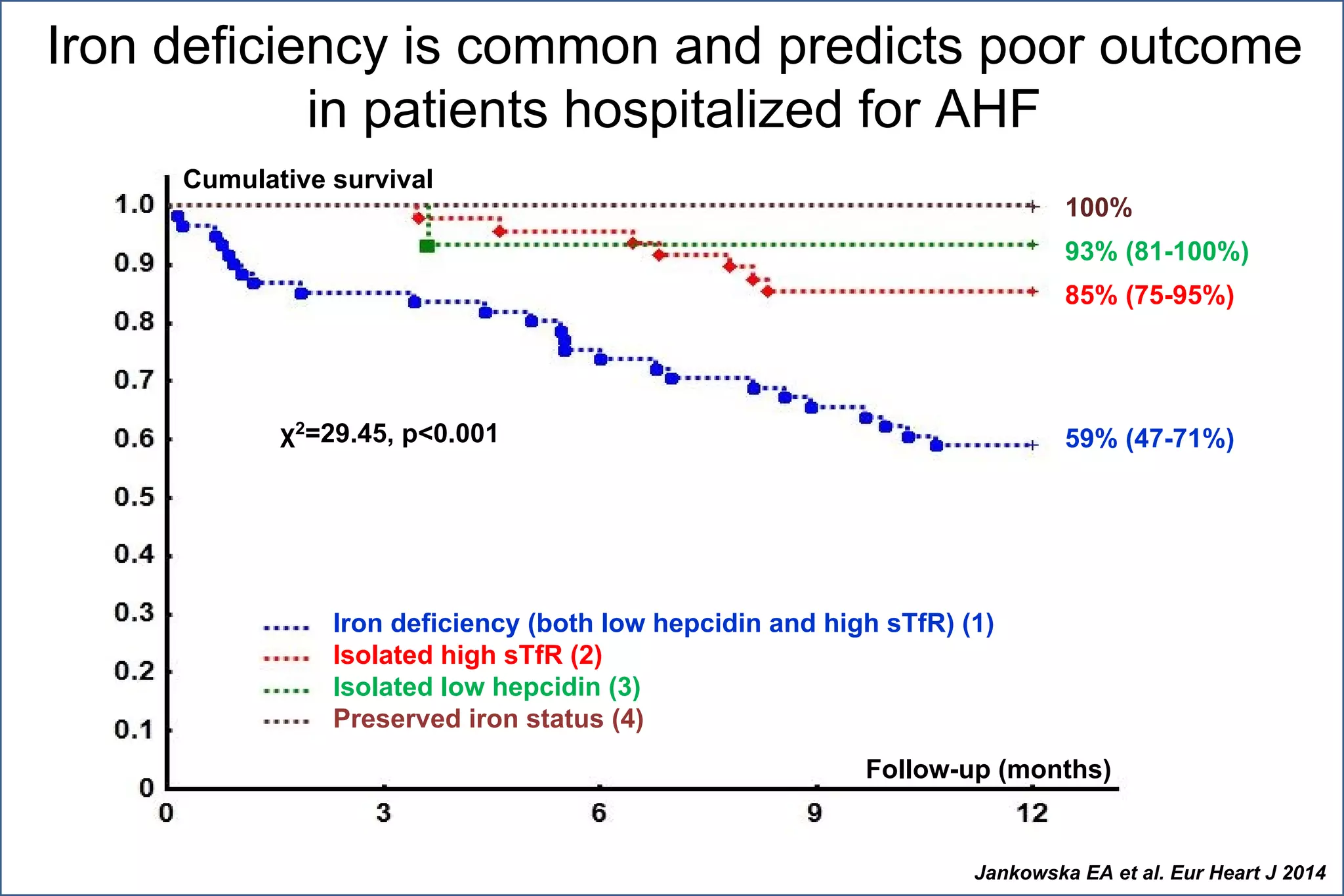
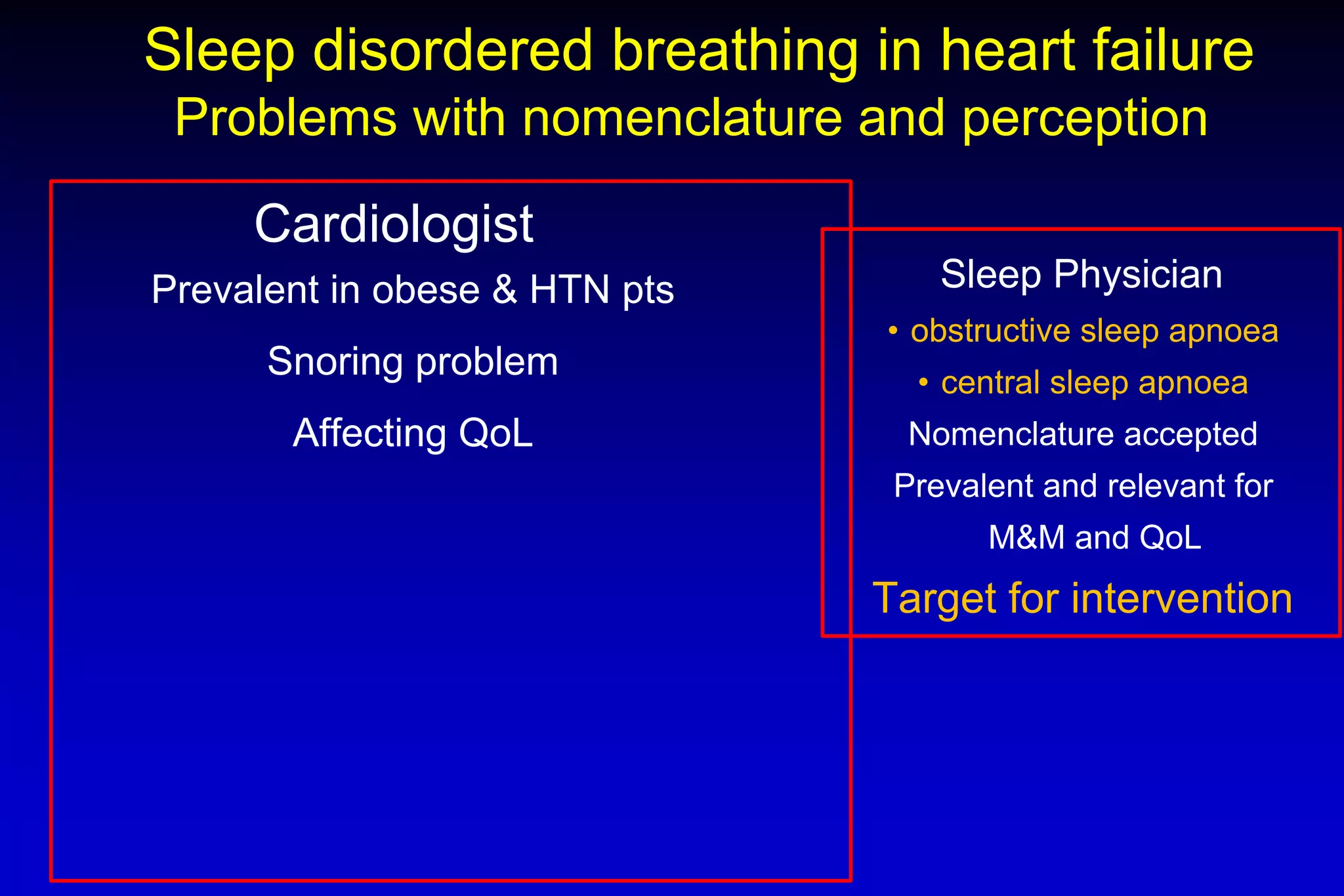
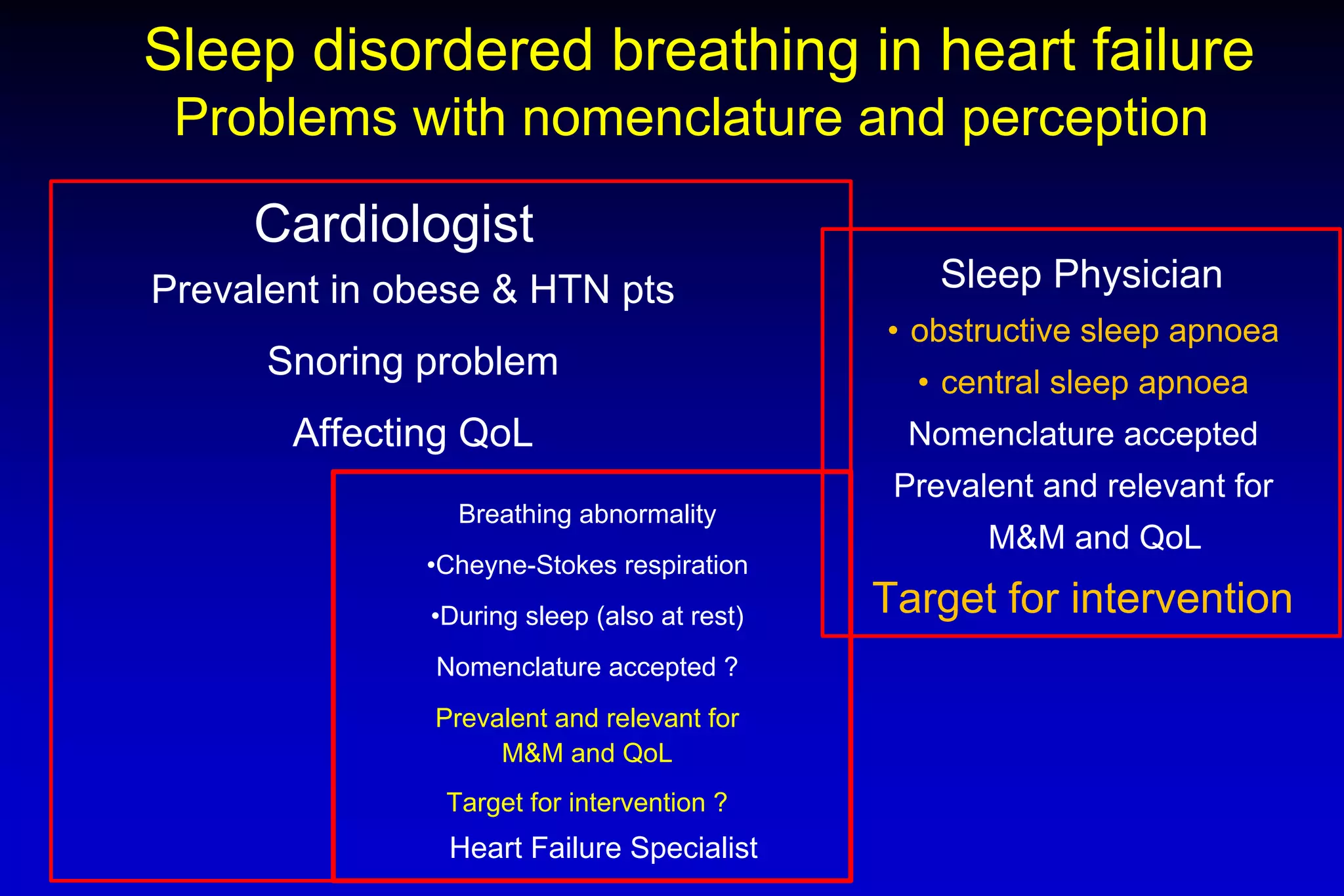
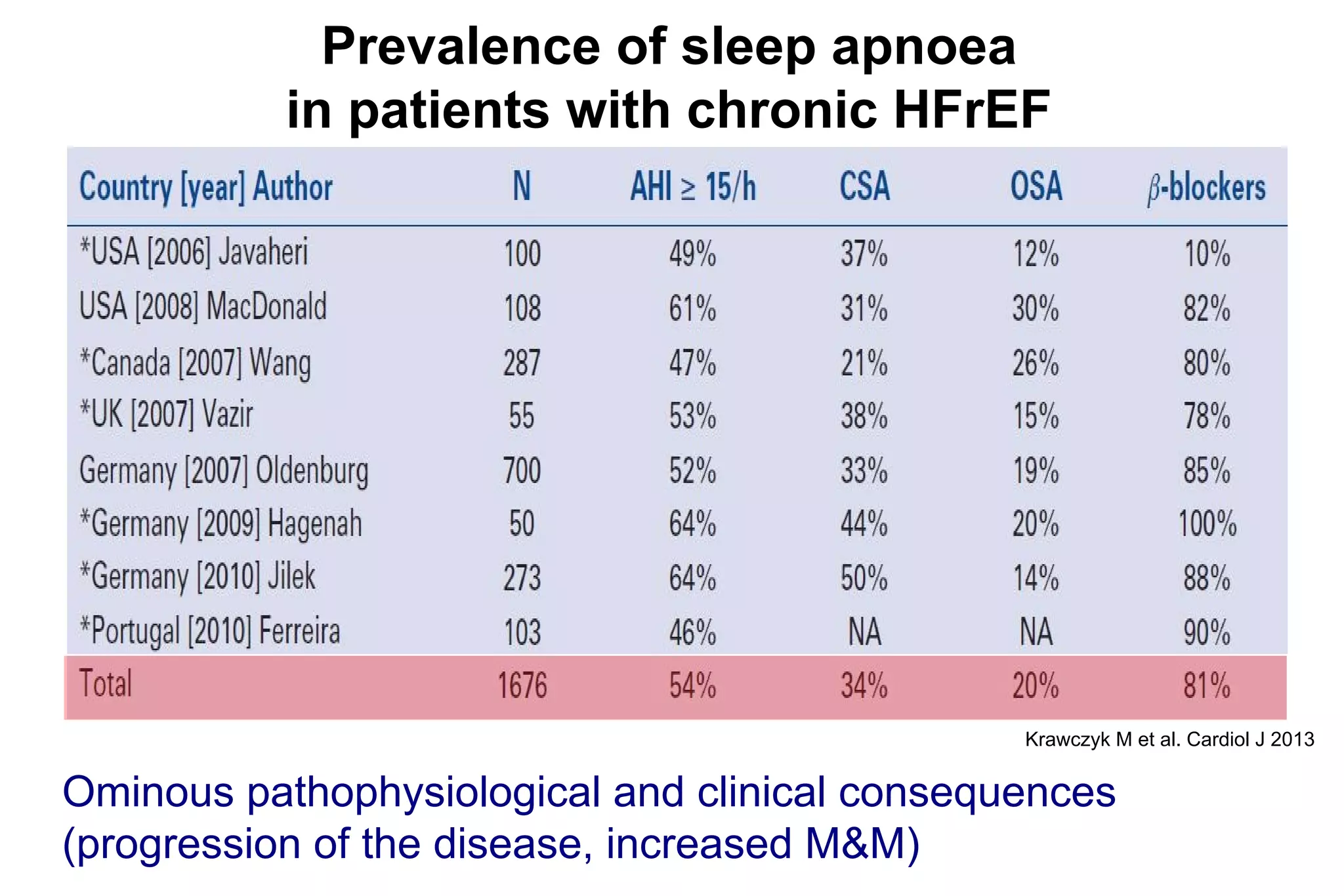
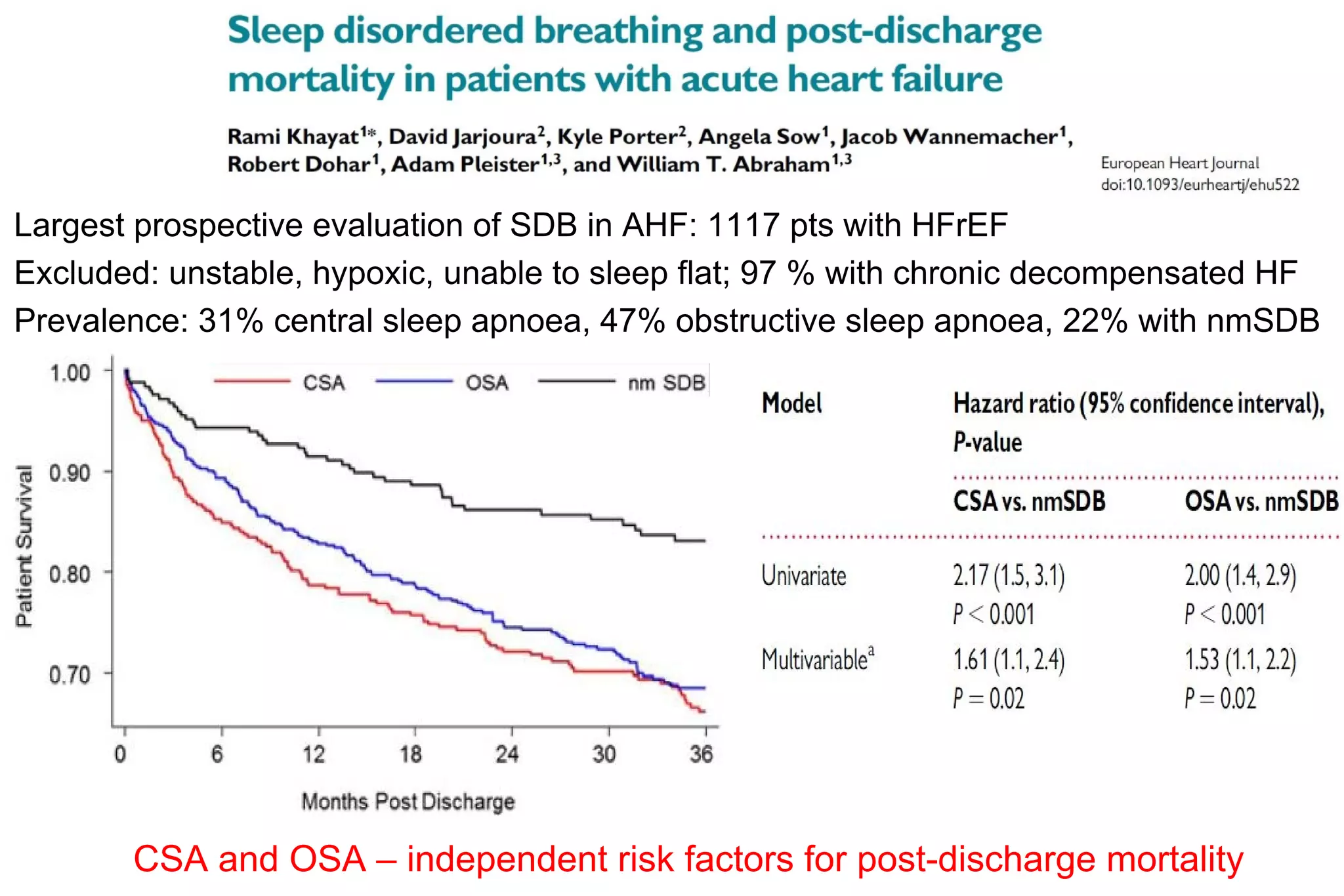
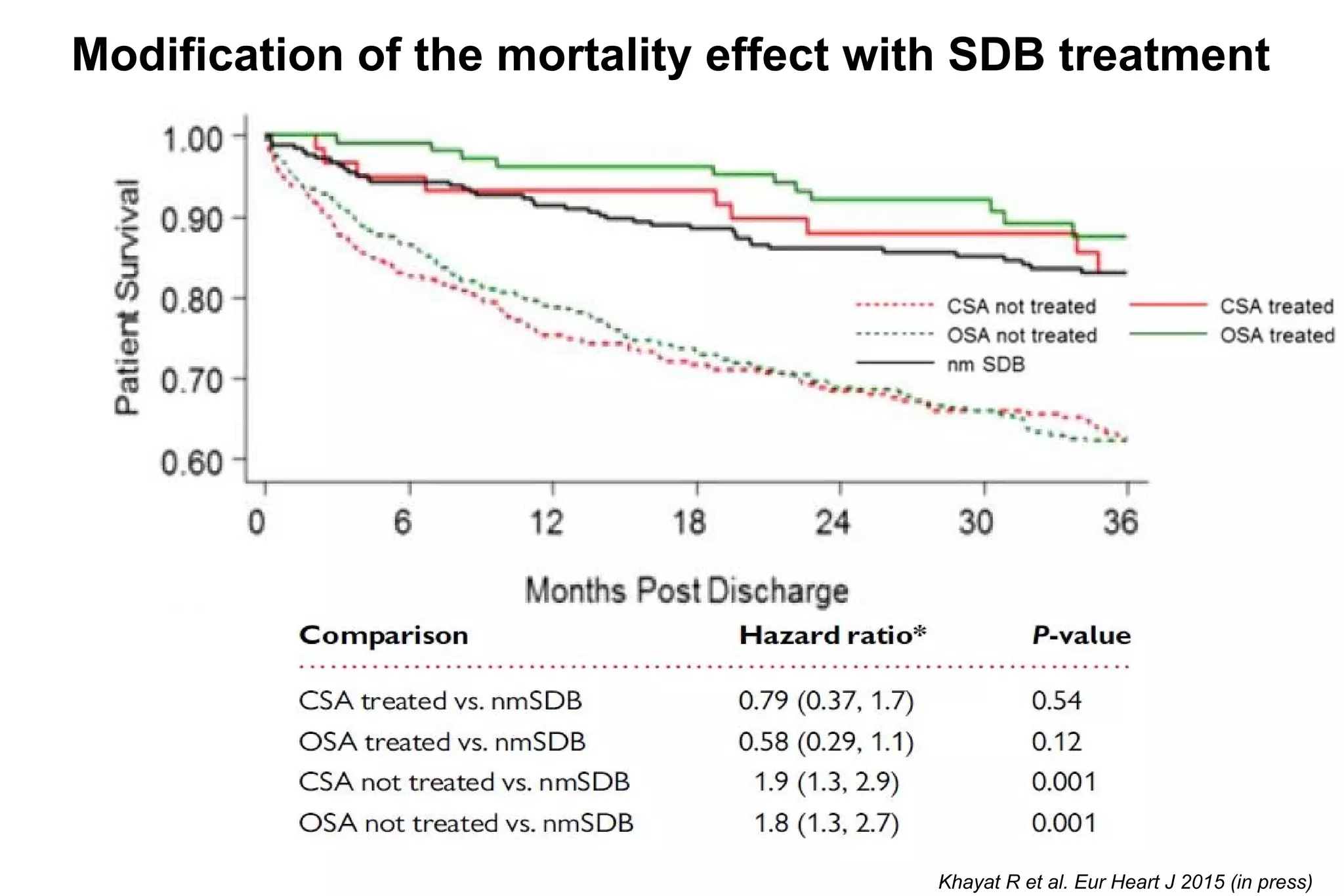
This document summarizes a presentation on cardiology topics including acute and advanced heart failure. It discusses trends in heart failure hospitalizations and mortality. It describes different hemodynamic profiles in acute heart failure patients and their corresponding treatments. It also discusses topics like iron deficiency in heart failure, sleep disordered breathing, and a study showing sleep disordered breathing is common in acute heart failure and predicts mortality.