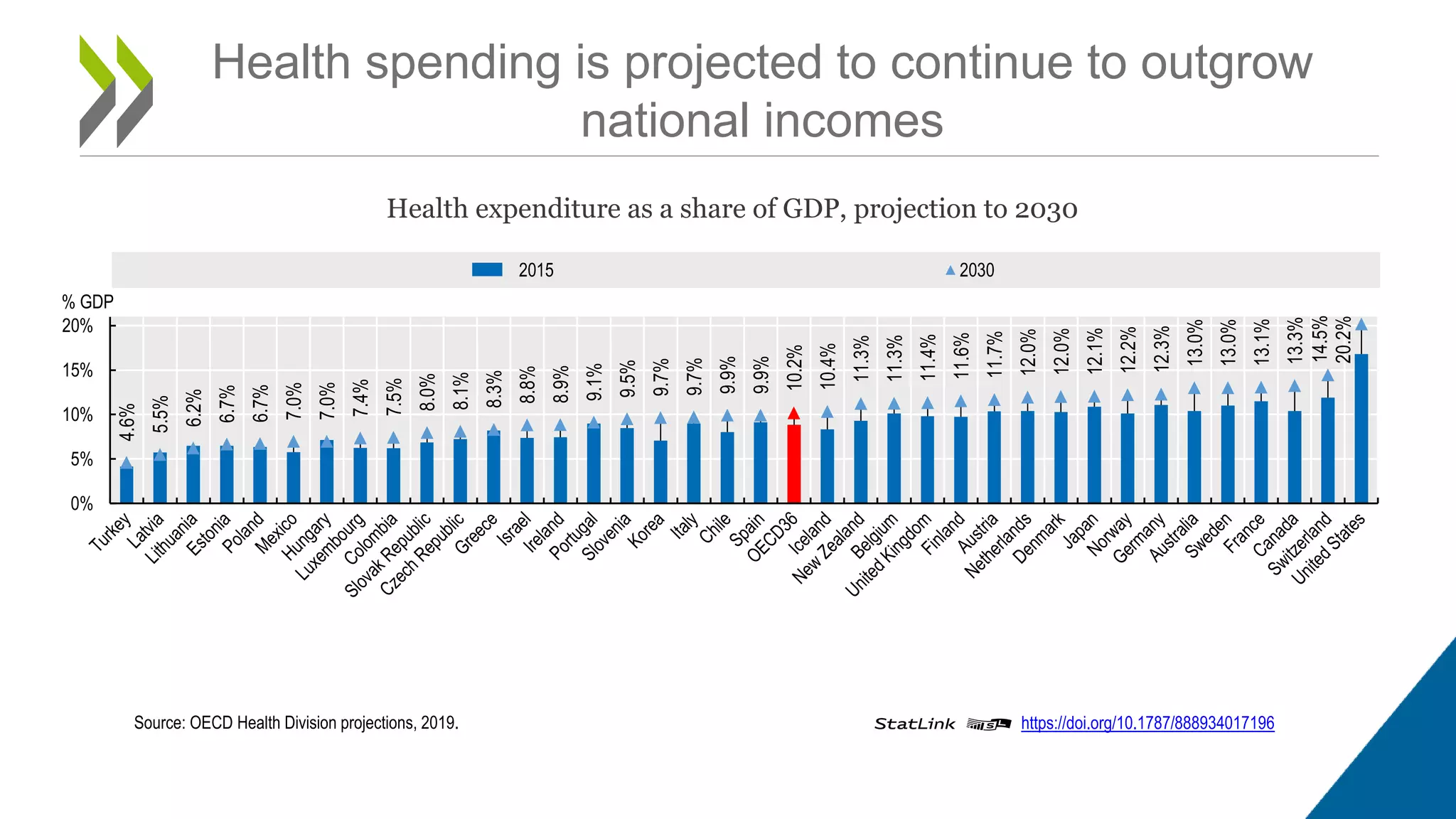
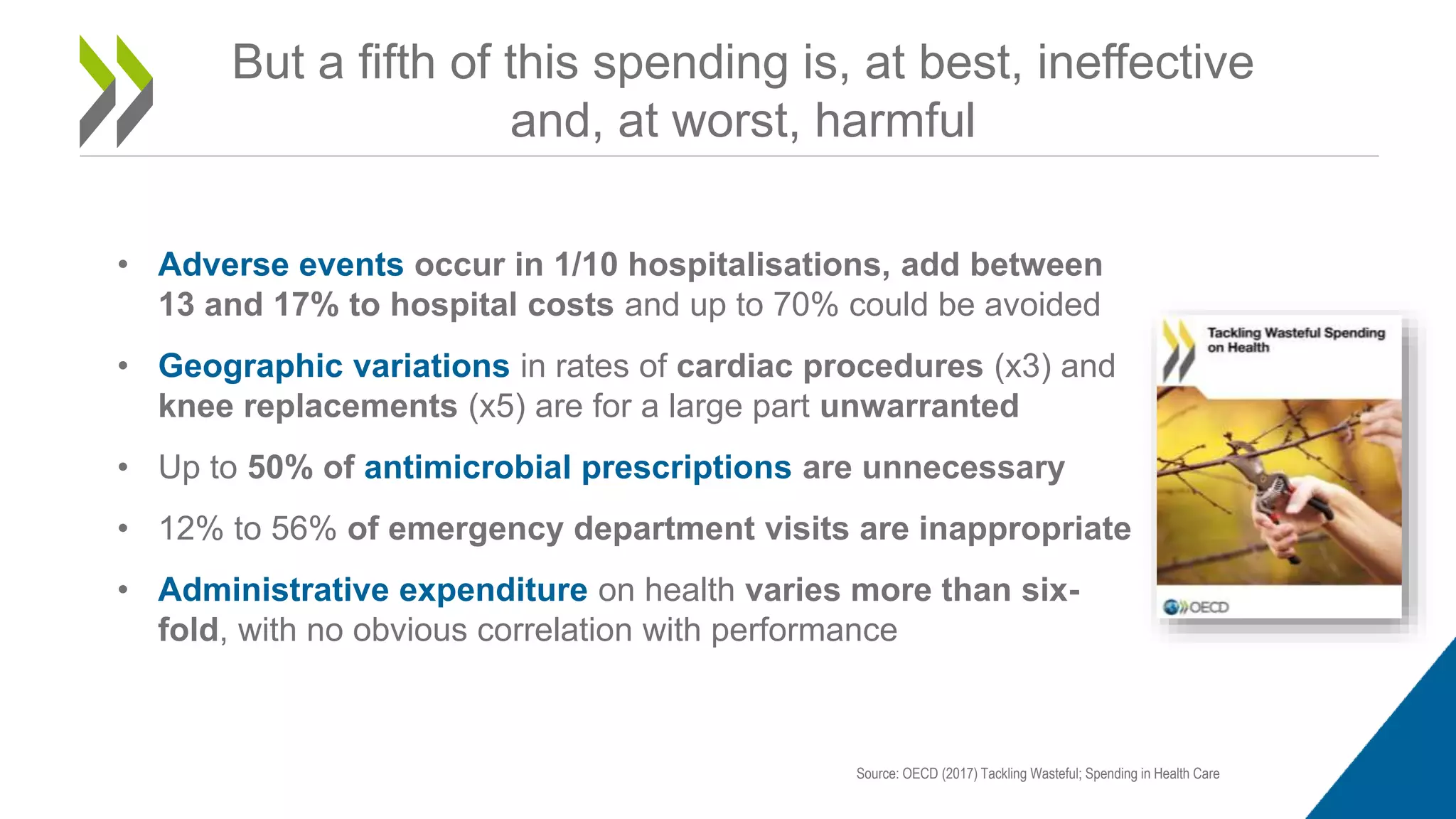
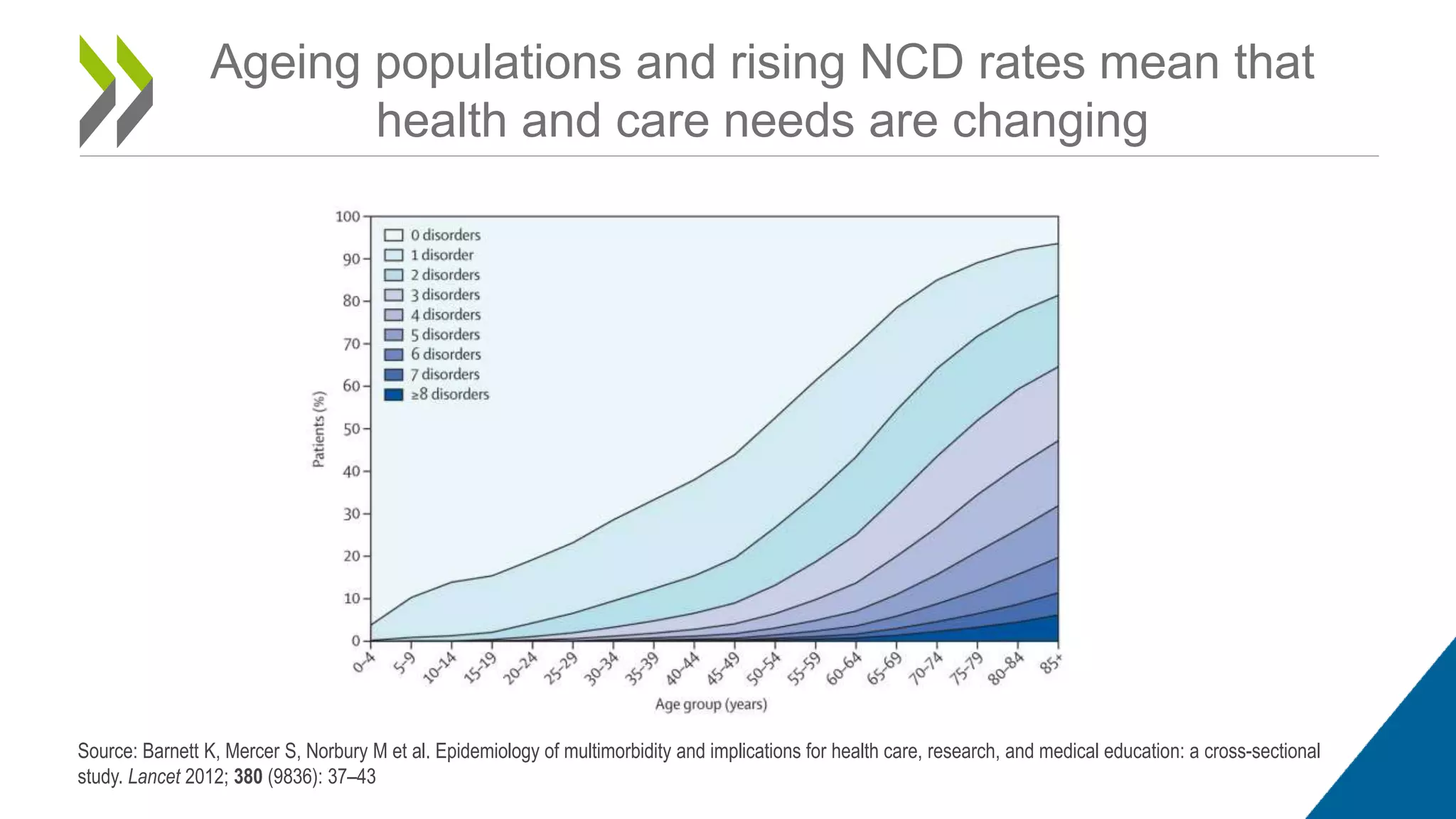
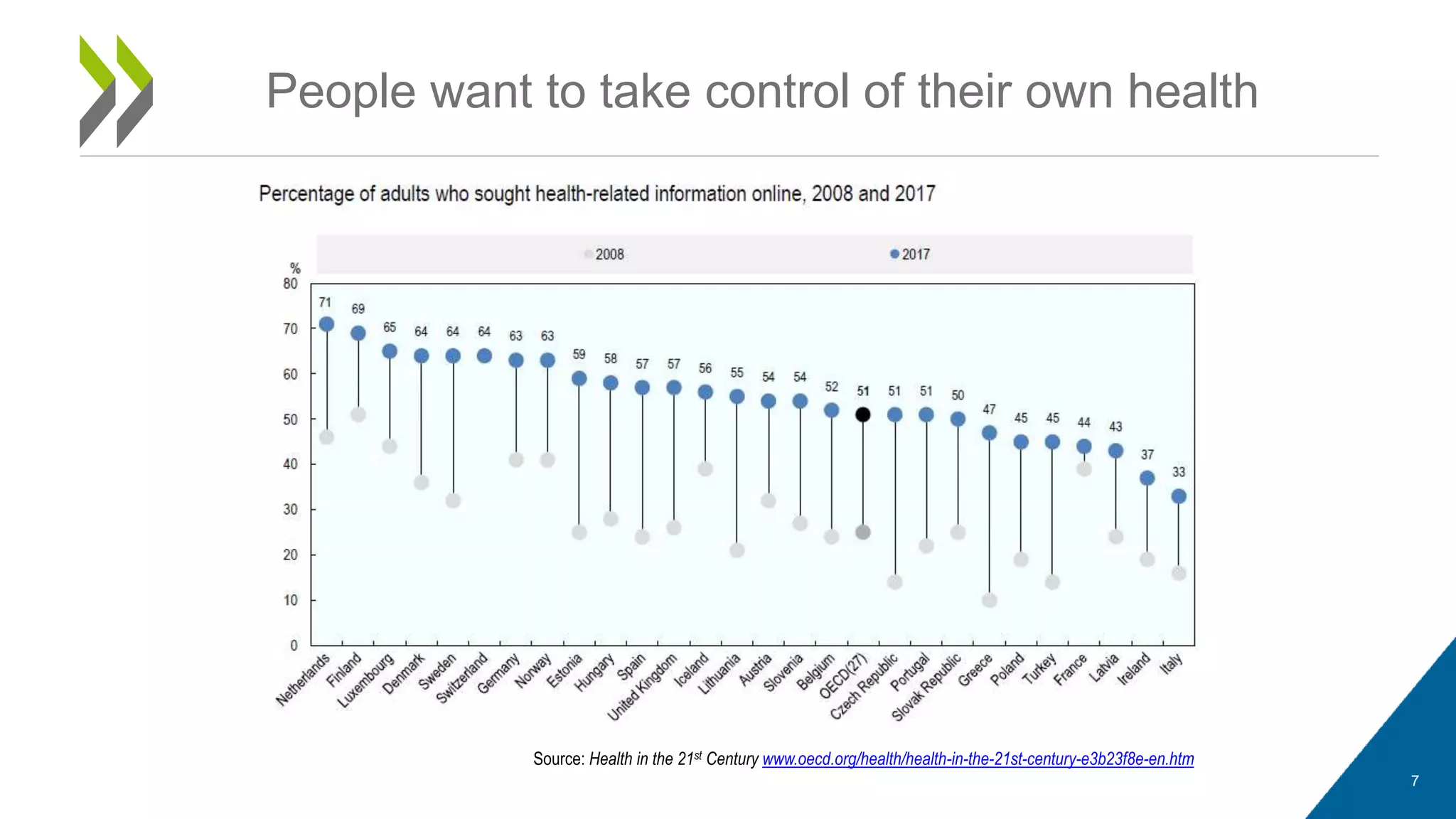
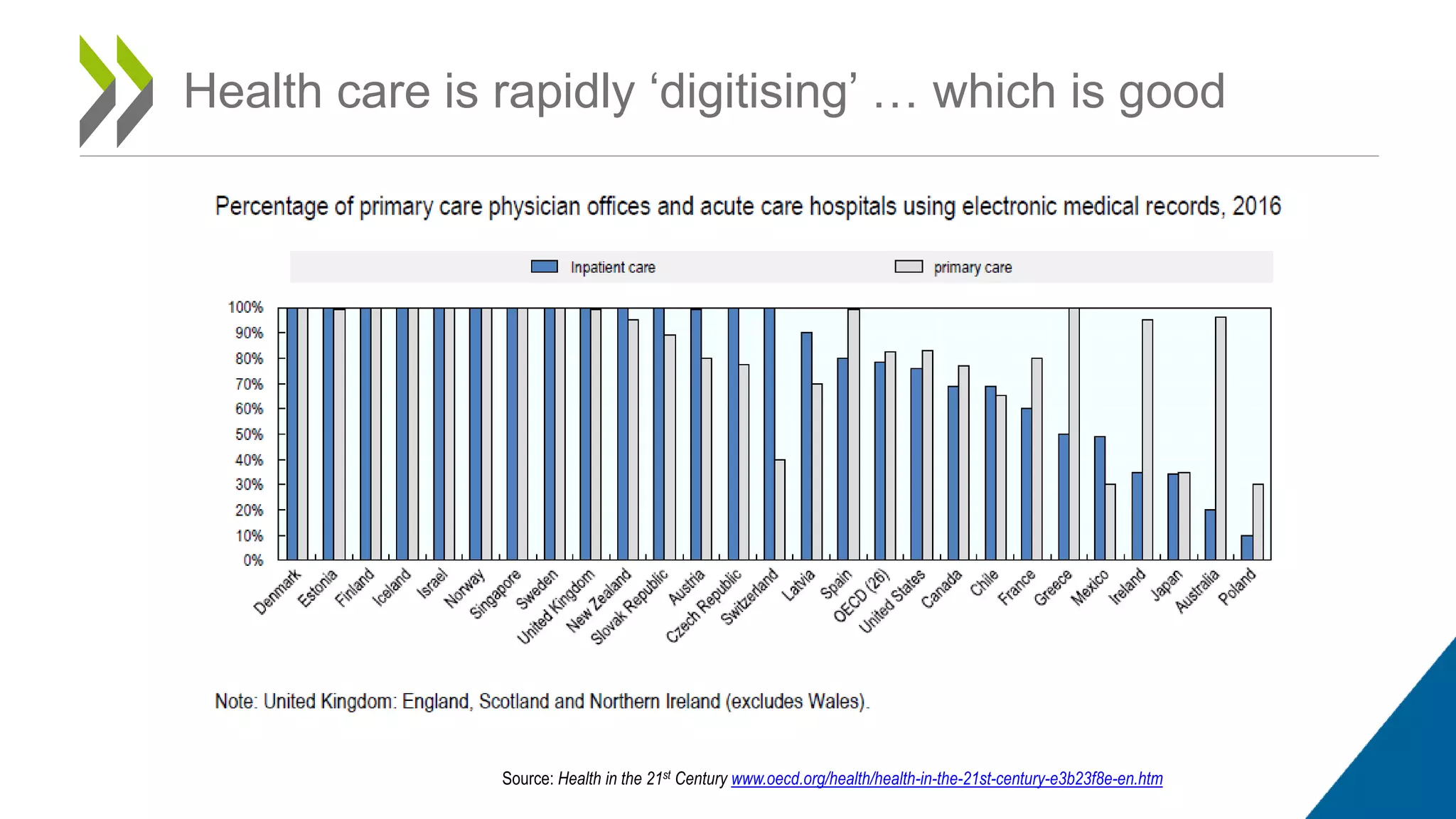
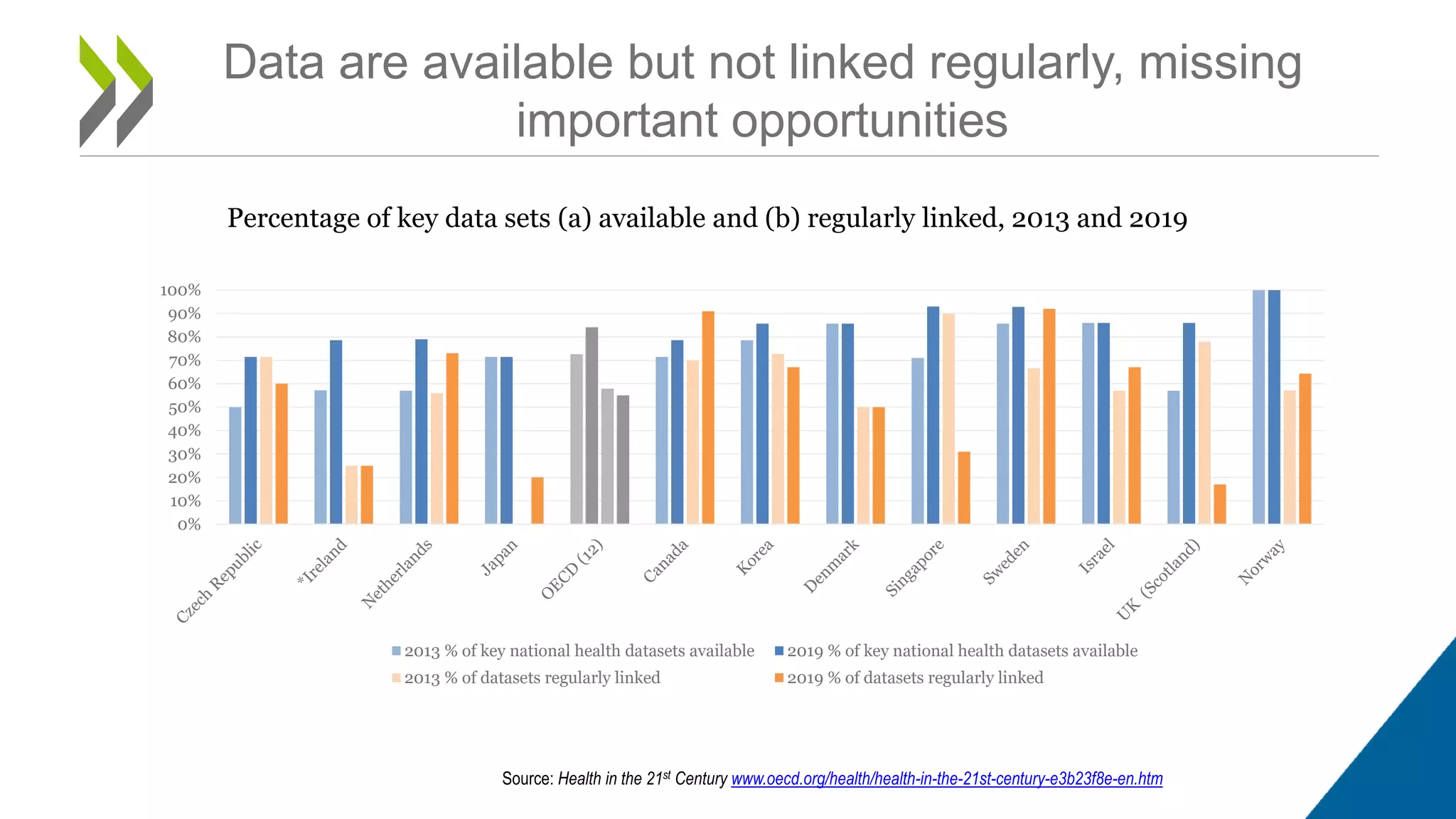
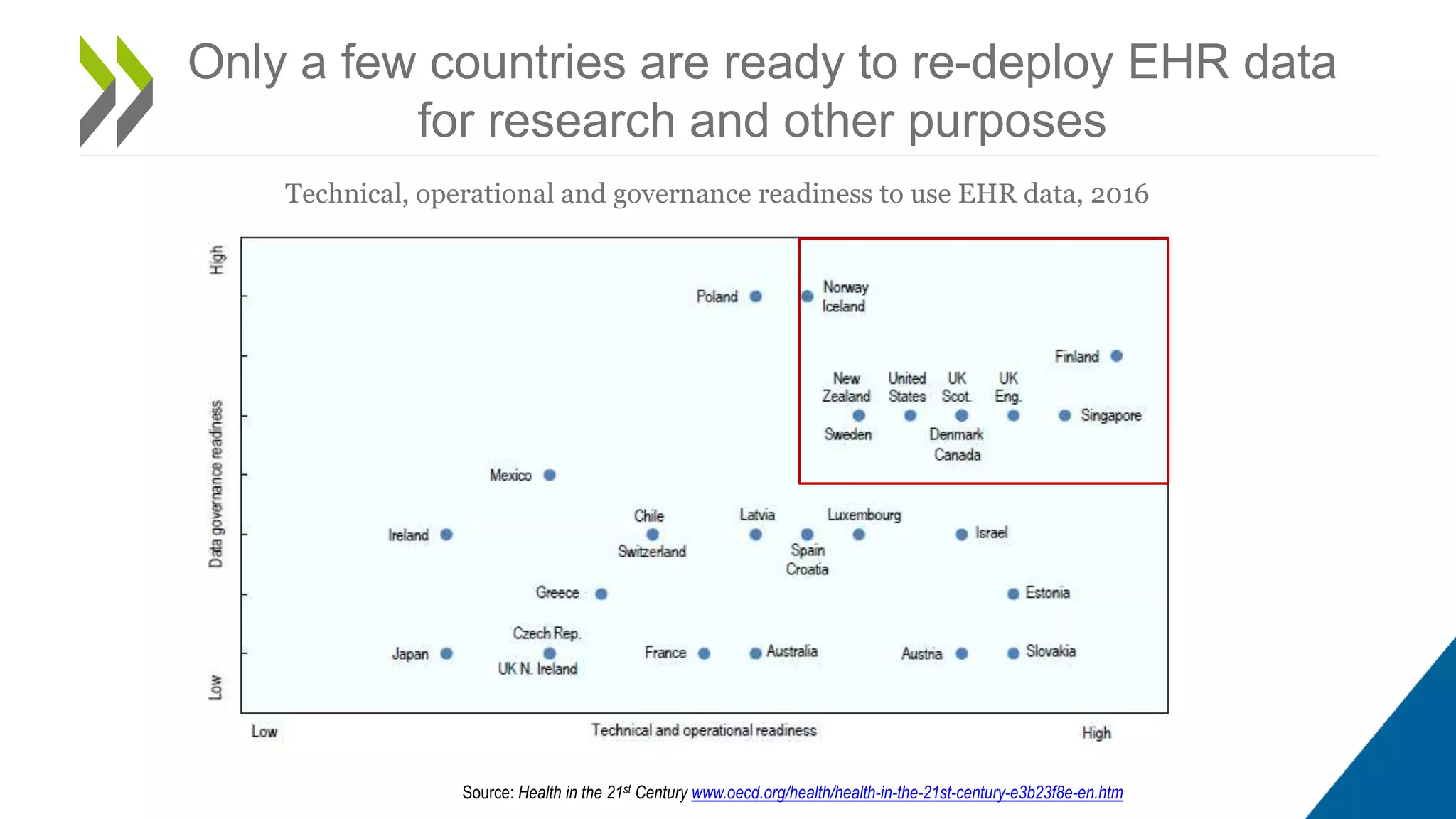
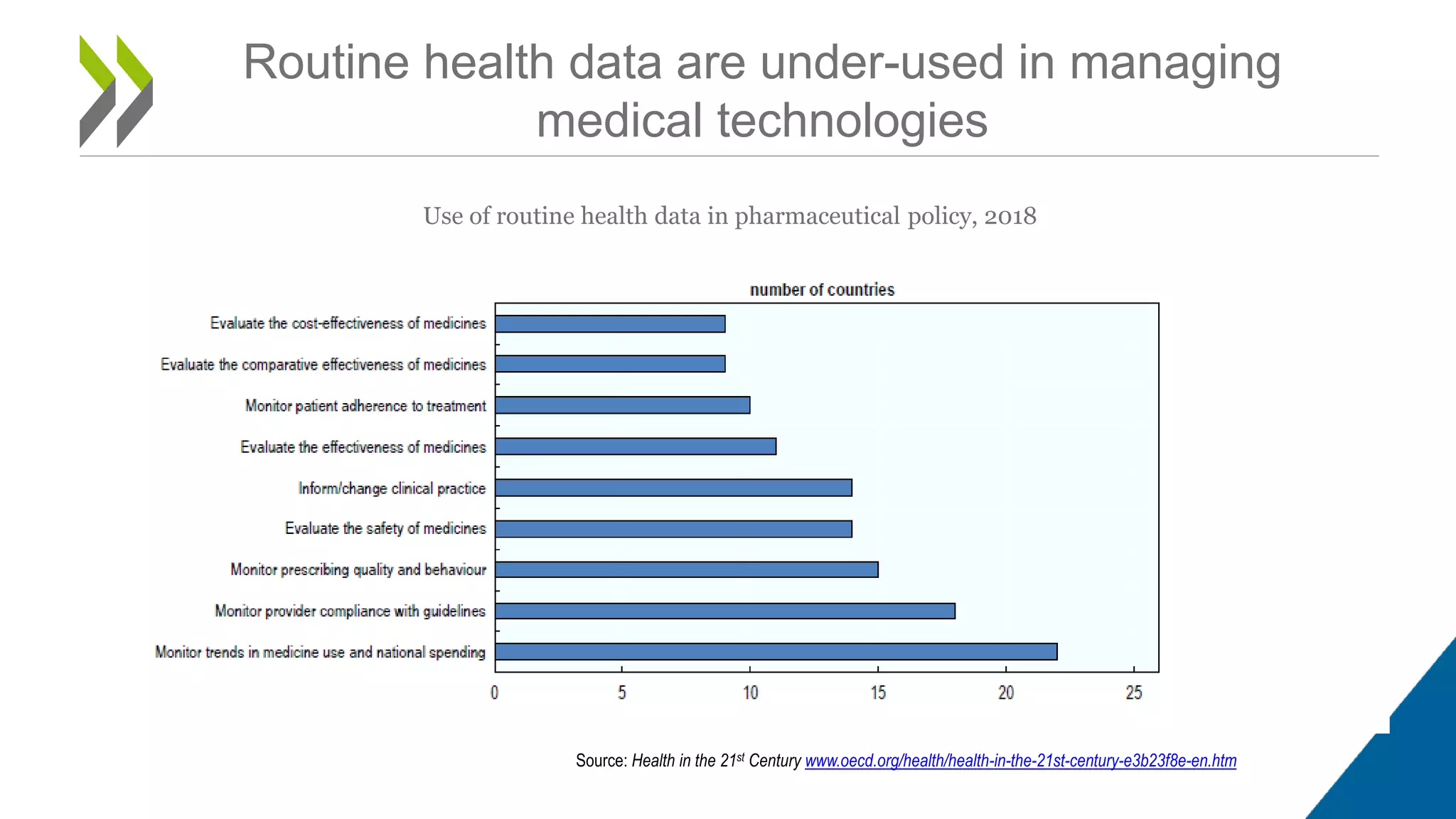
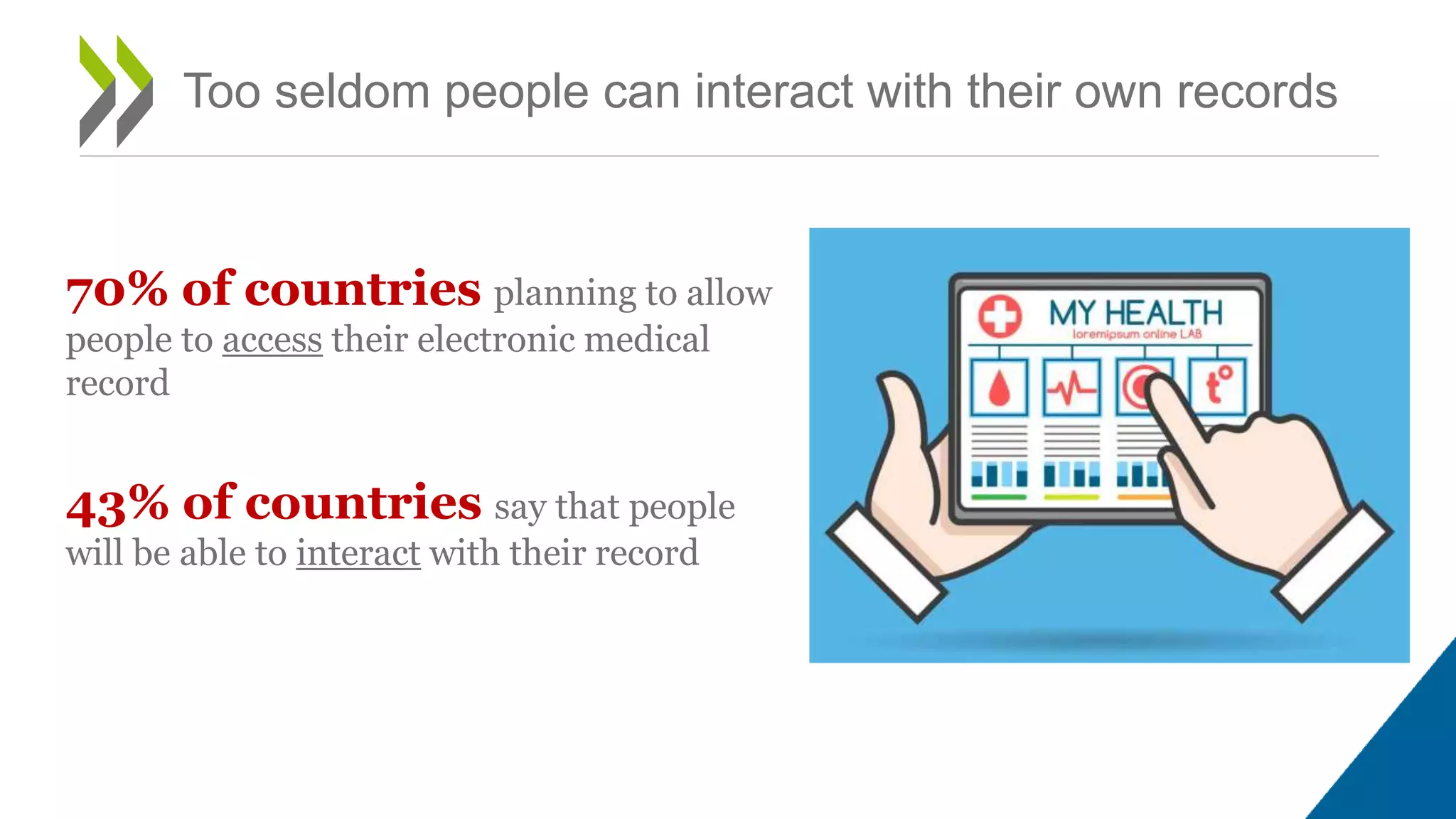
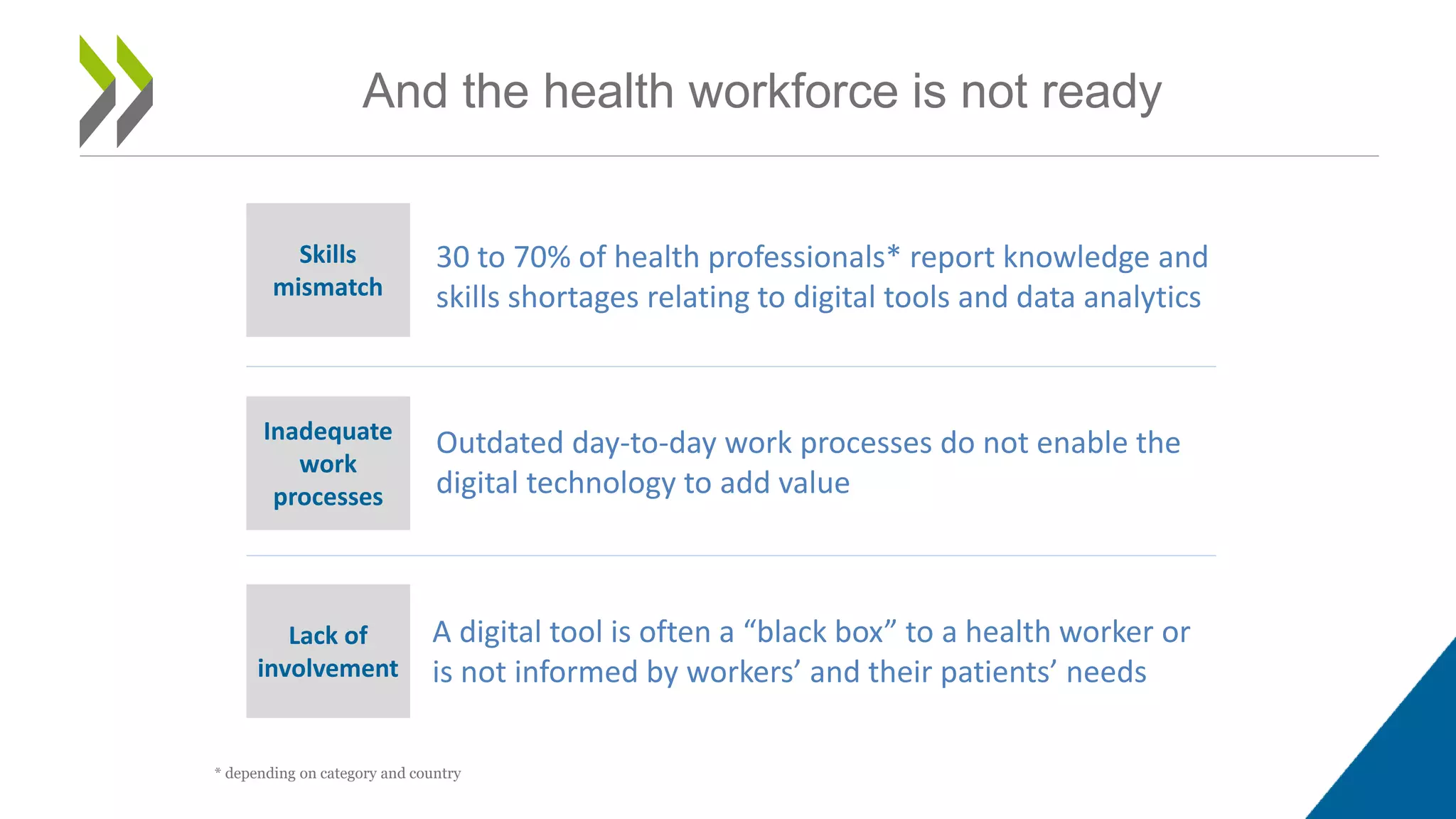
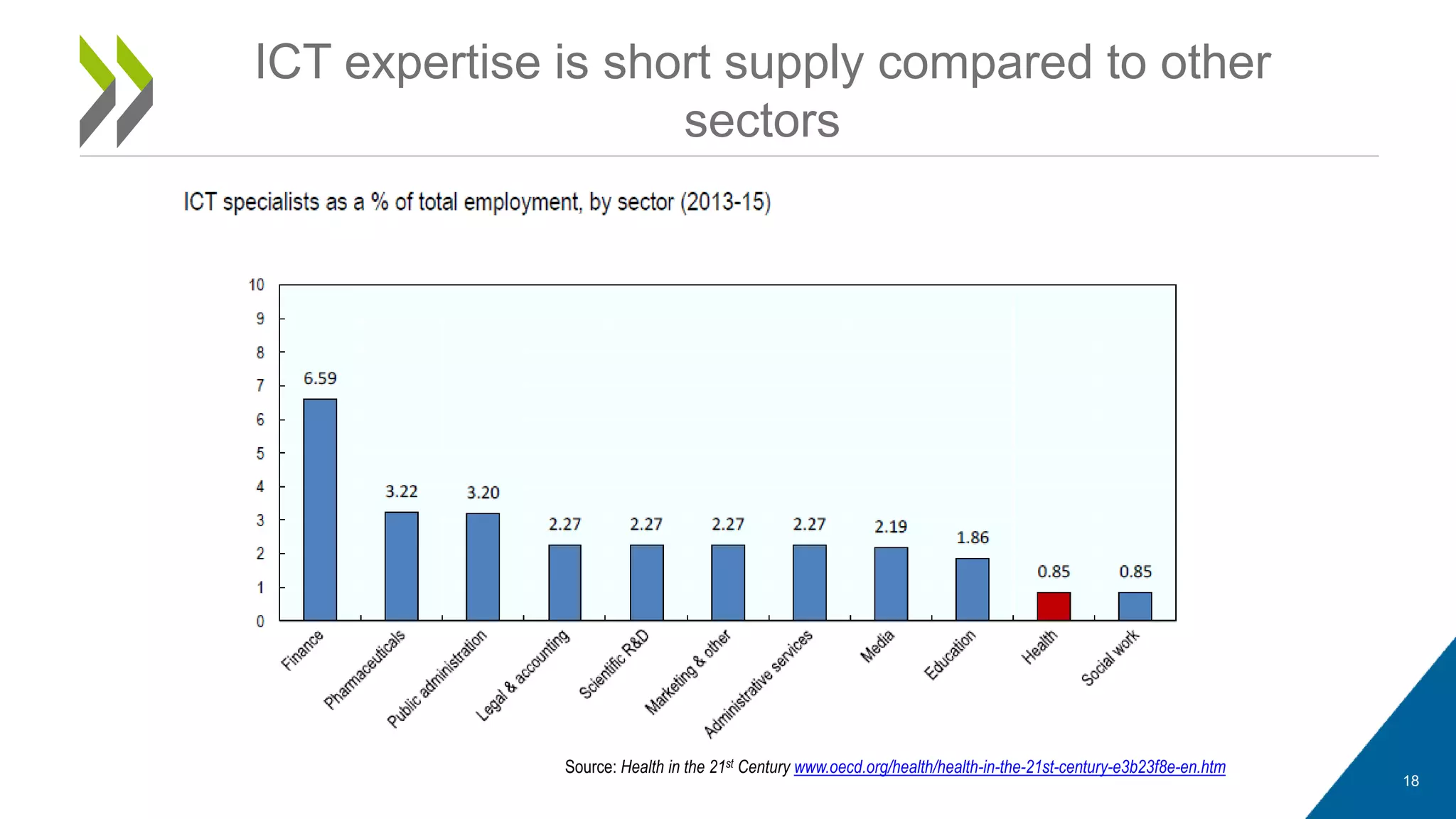
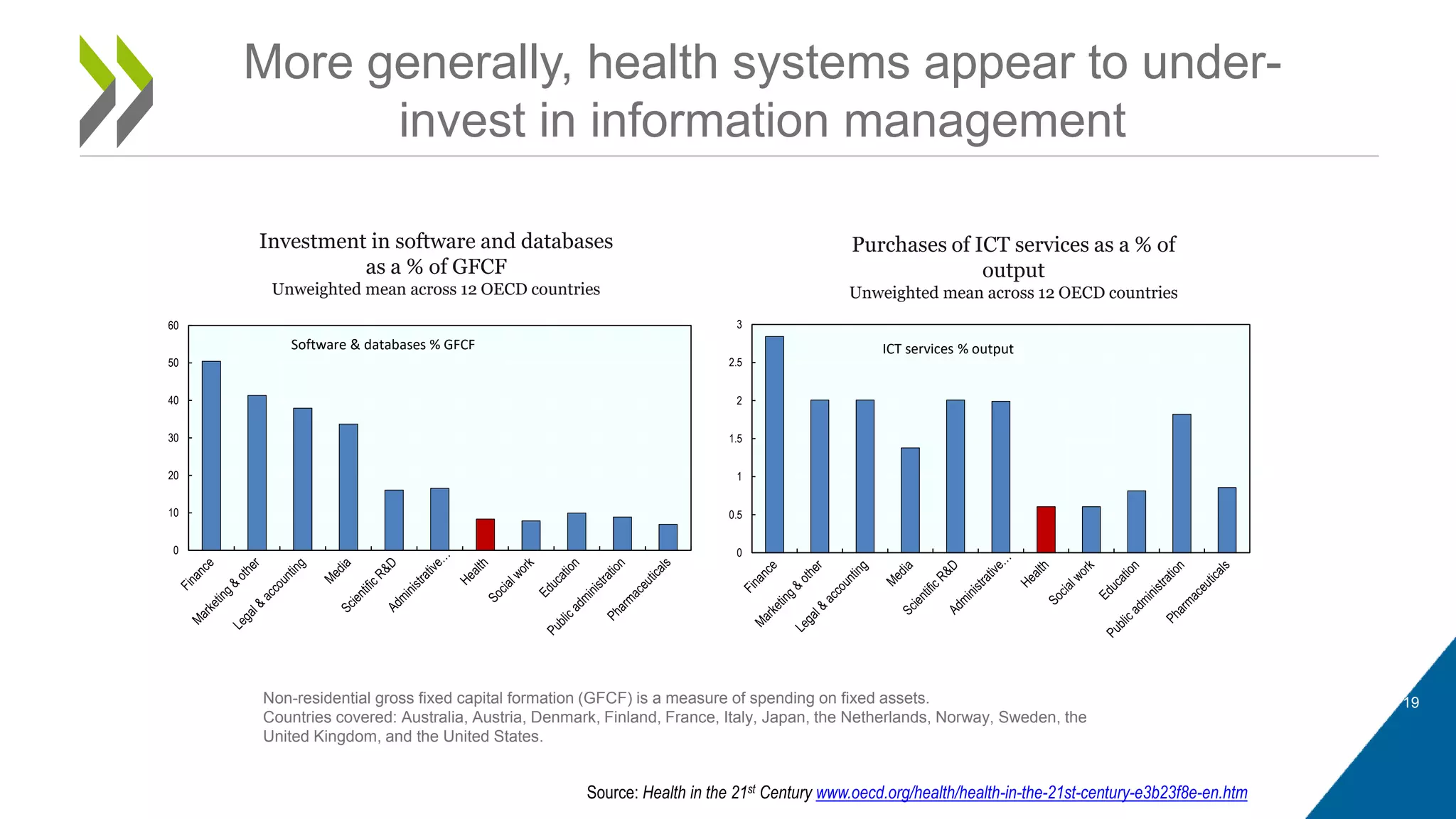
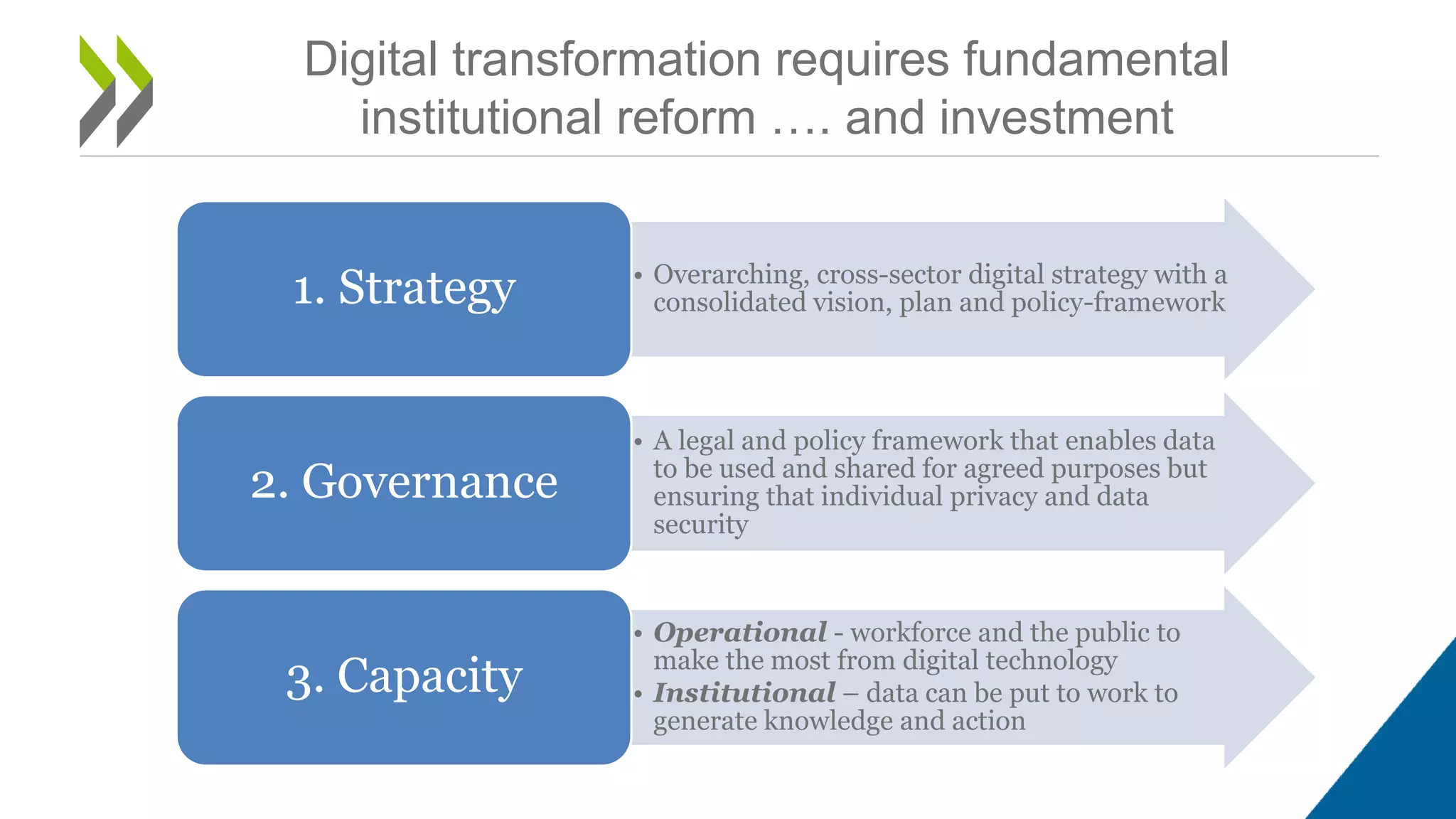
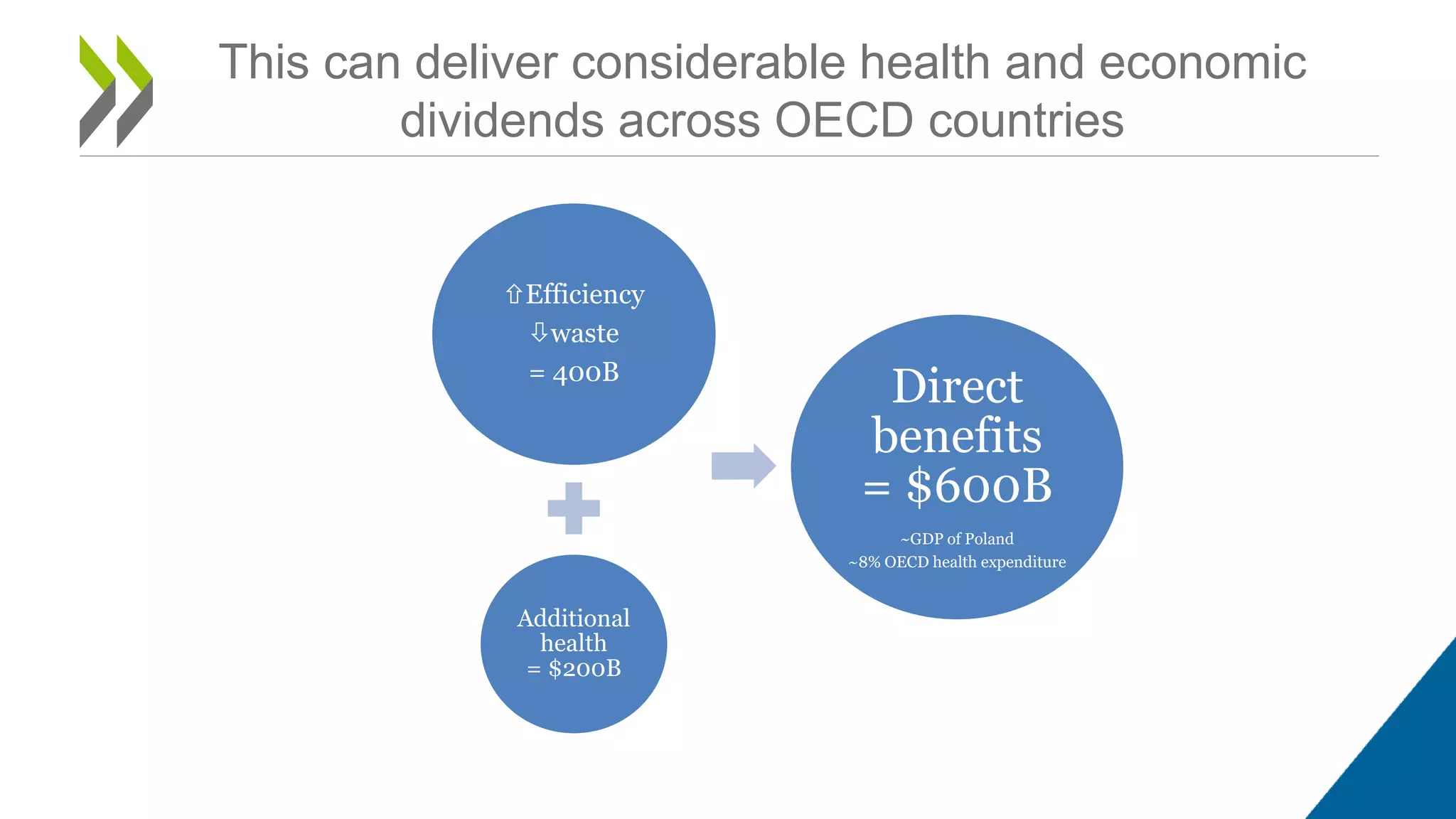
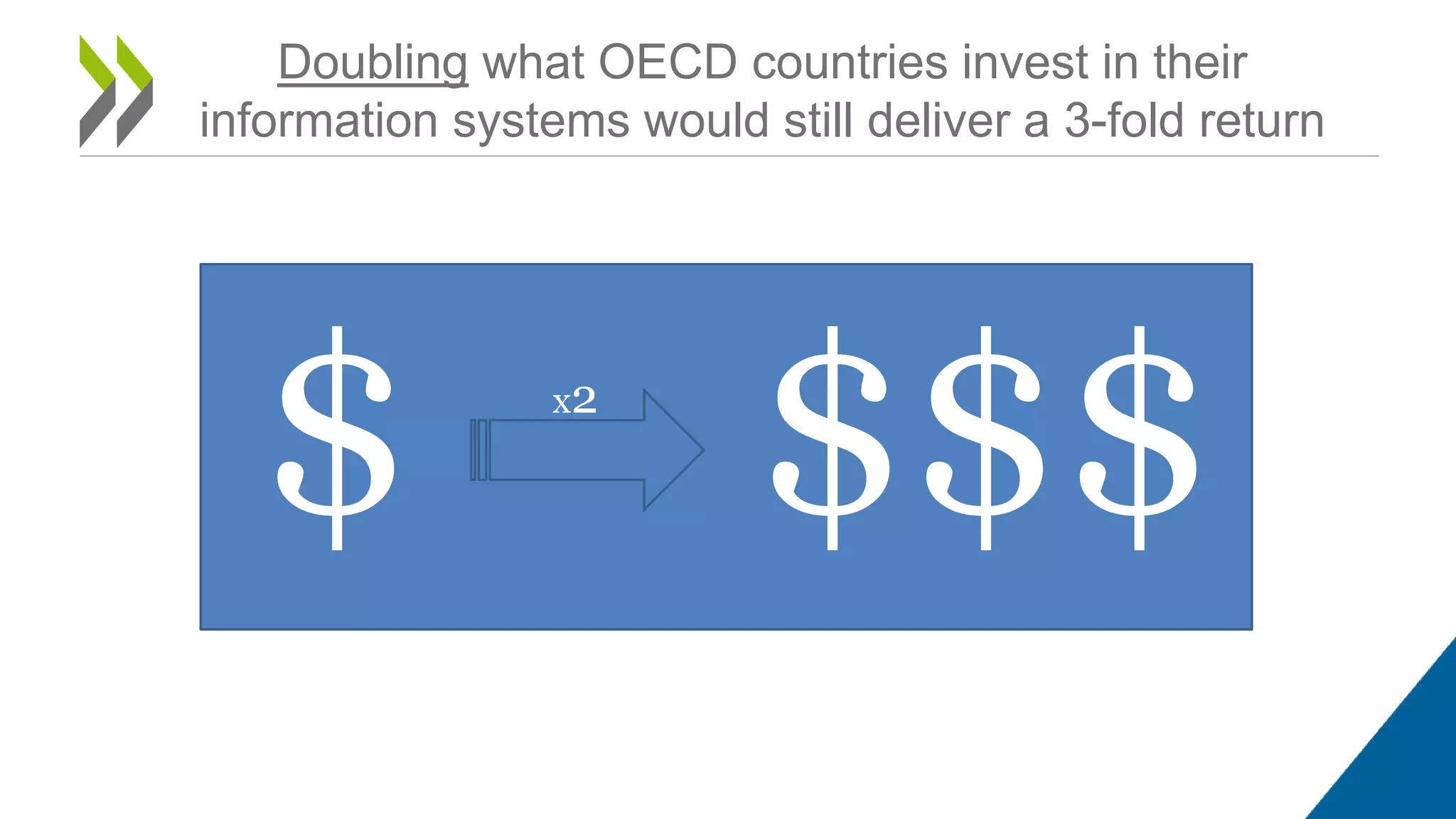
The document discusses the evolving challenges and opportunities in health systems in the 21st century, highlighting the increasing healthcare spending and inefficiencies within the current systems. It emphasizes the potential of data and digital technology to enhance healthcare delivery, optimize management, and improve patient involvement, while also indicating that many health systems remain underprepared for digital transformation. Overcoming institutional barriers and investing in information management are crucial for leveraging digital tools effectively.