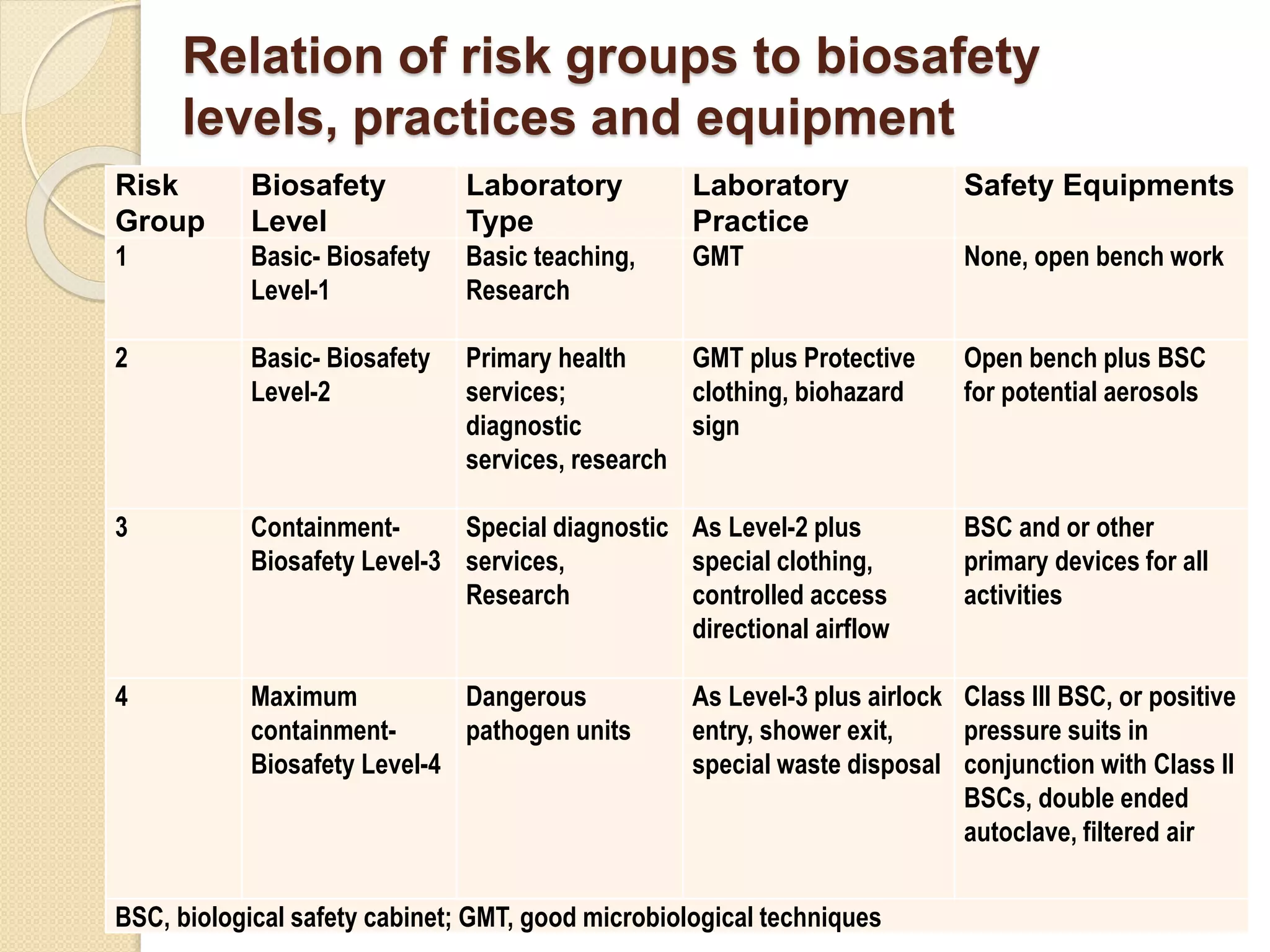
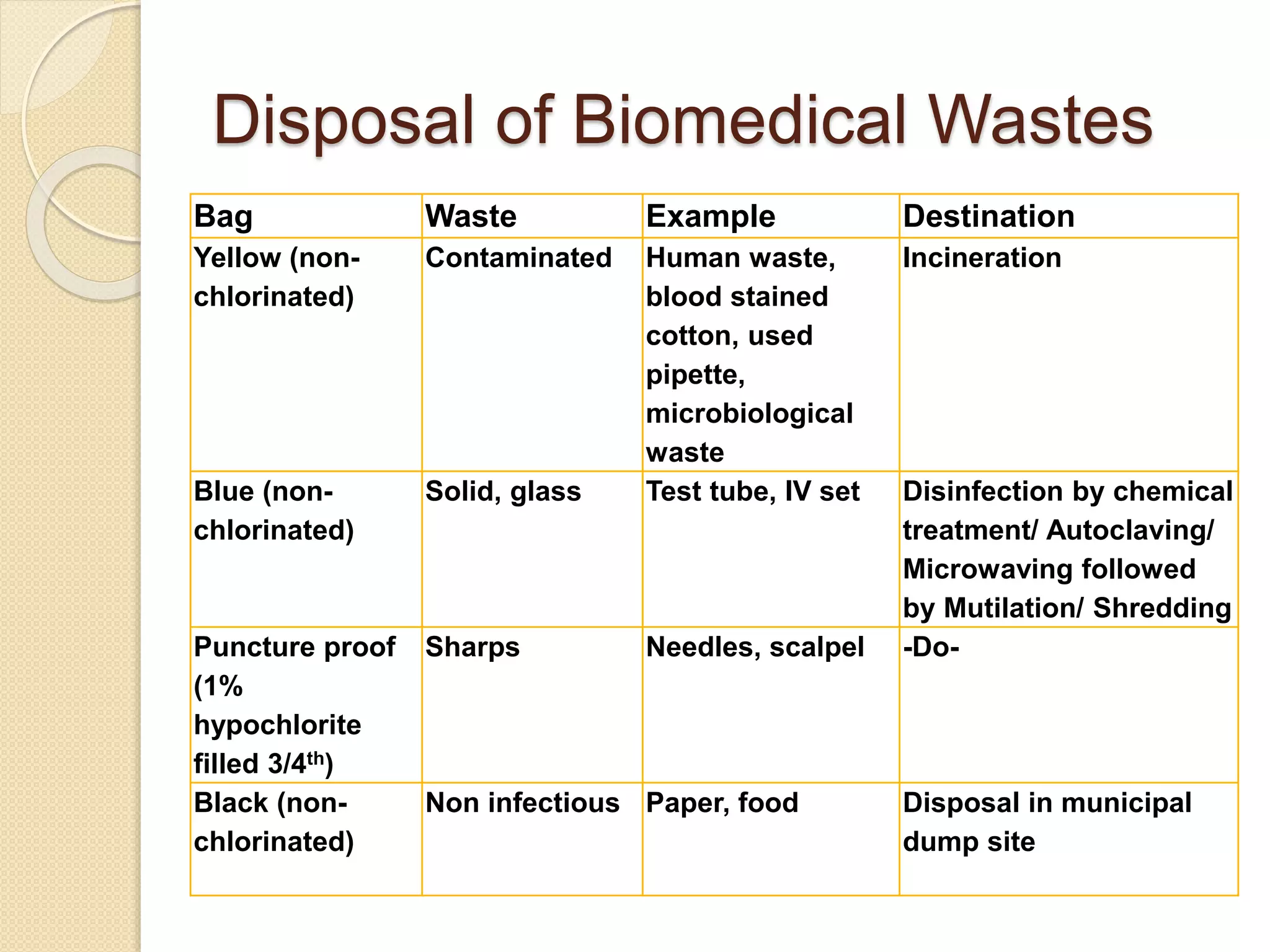
The document discusses health and safety practices in microbiological laboratories. It covers topics such as risk group classification of pathogens, biosafety levels and practices, selection and use of biological safety cabinets, personal protective equipment, hand hygiene, needlestick injuries, laboratory spill management, biomedical waste disposal, and fire hazards. The key points are that pathogens are classified into four risk groups based on individual and community risk levels, and appropriate biosafety levels, practices and equipment are selected according to the risk group to minimize hazards.