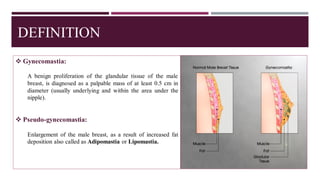
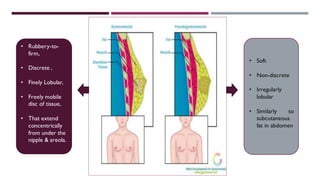
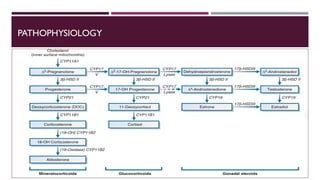
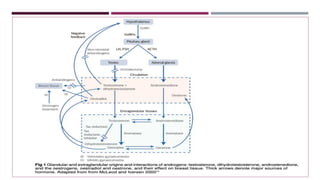
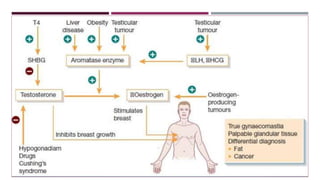
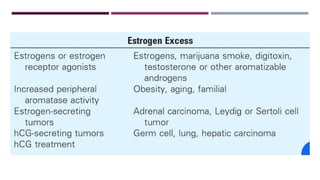
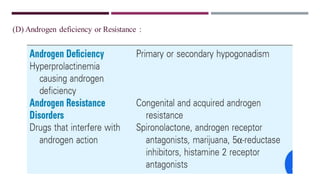
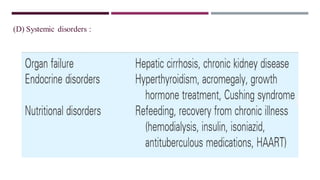
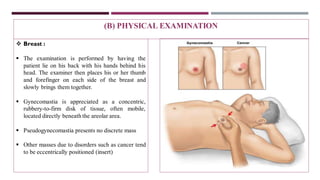
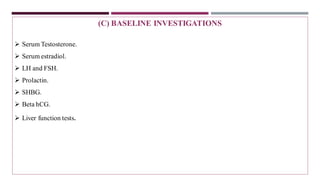
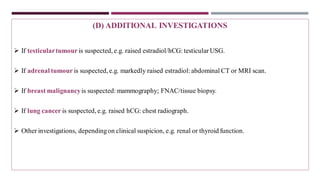
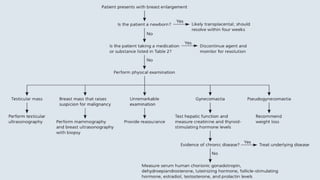
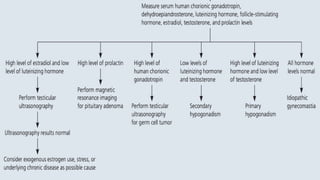
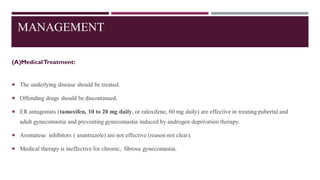
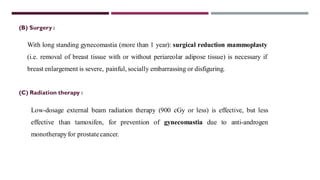
Gynecomastia is a benign proliferation of glandular breast tissue in males. It results from an imbalance of estrogen and androgen levels. Common causes include physiological changes during puberty or aging, as well as medical conditions or medications that influence hormone levels. Evaluation involves medical history, physical exam, and hormone level testing. Mild or temporary cases may resolve on their own or with tamoxifen treatment, while surgery is recommended for chronic or severe gynecomastia.