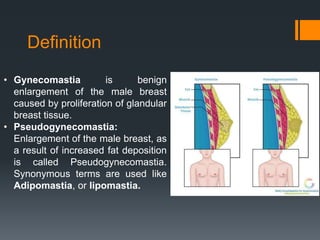
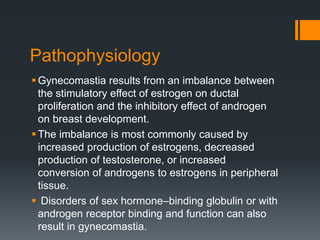
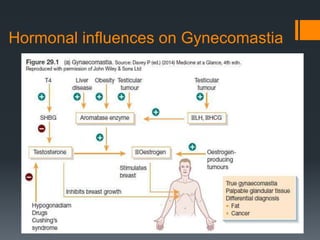
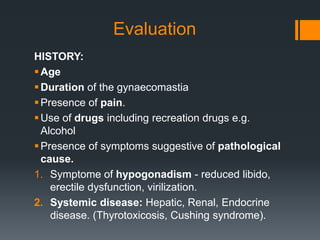
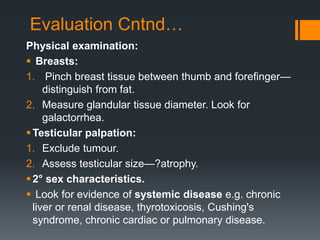
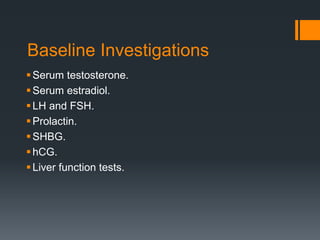
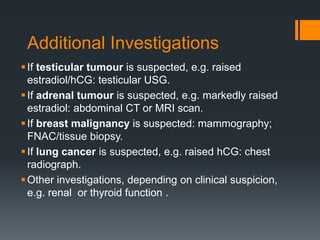
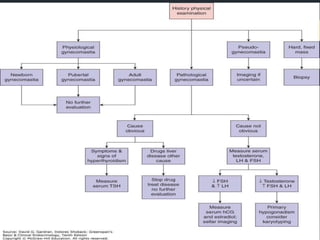
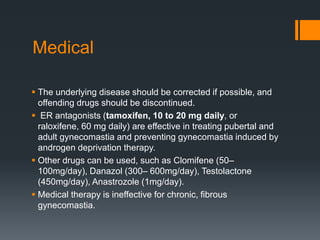
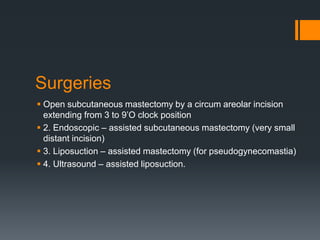
Gynecomastia is the benign enlargement of breast tissue in males caused by a hormonal imbalance with increased estrogen or decreased androgen levels. It can occur physiologically during puberty, aging or due to certain drugs. Evaluation involves history, exam and blood tests to check hormone levels and rule out underlying causes. Treatment depends on the severity and cause, with medical management using tamoxifen or surgery to remove breast tissue for longstanding or severe cases. Complications of surgery can include nipple or skin issues.