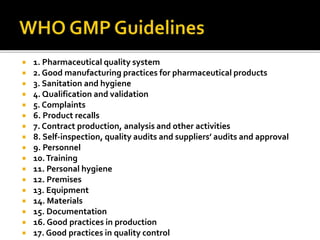
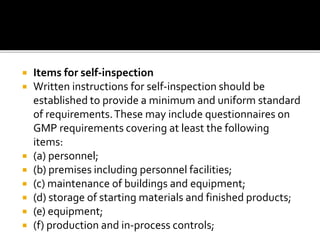
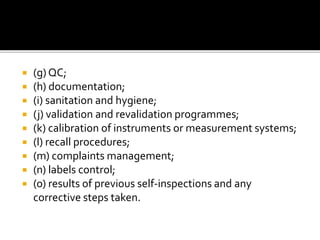
The document outlines WHO guidelines for good manufacturing practices (GMP) in the pharmaceutical industry. It discusses how GMP ensures quality control throughout the production process, from procurement of materials to finished products. Key aspects covered include facilities and equipment qualification, sanitary conditions, documentation practices, personnel training, and quality control testing. Adhering to GMP is important for minimizing risks and ensuring patient safety.