This document provides an overview of ICH E6(R1) guidelines for good clinical practice. The key points are:
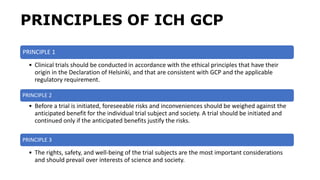
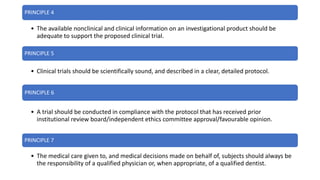
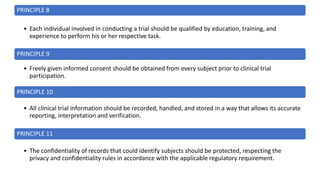
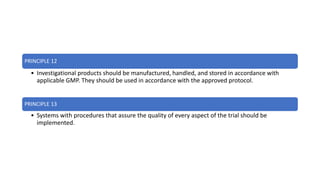
1. ICH E6(R1) provides ethical and quality standards for clinical trial design, conduct, recording and reporting to protect subject rights and ensure data credibility.
2. The guidelines aim to harmonize standards across Europe, Japan and the US to facilitate mutual acceptance of clinical data by regulatory authorities.
3. The document outlines principles like prioritizing subject safety, obtaining informed consent, and ensuring trial conduct follows approved protocols.
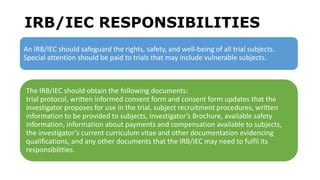
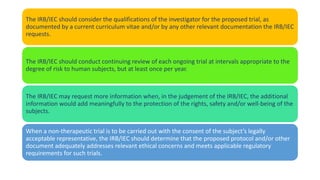
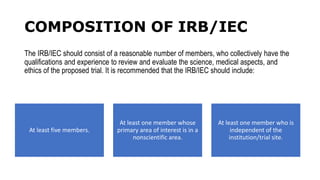
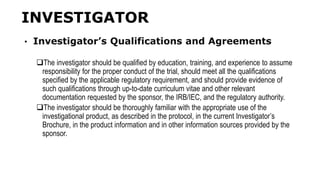
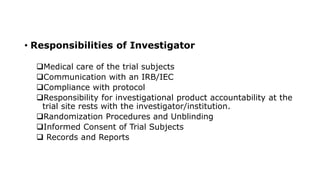
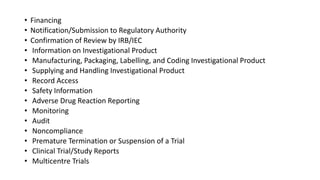
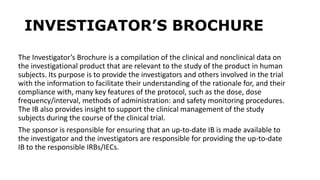
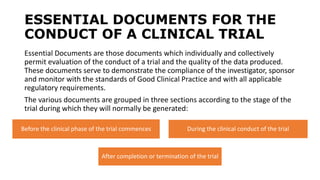
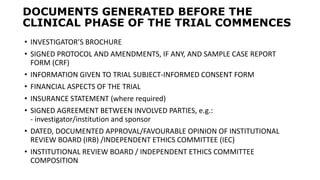
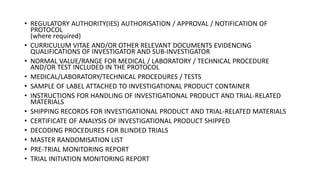
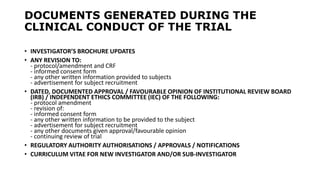
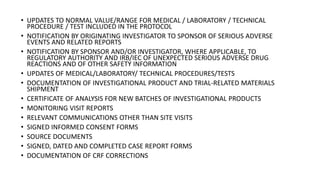
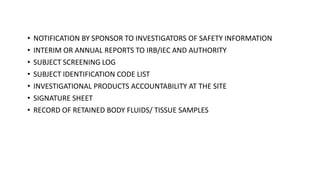
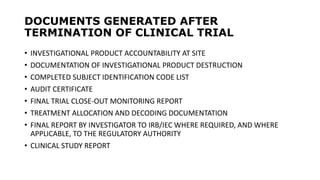
4. It also describes responsibilities of parties involved like investigators, sponsors, and ethics committees. Proper documentation and oversight are important to demonstrate