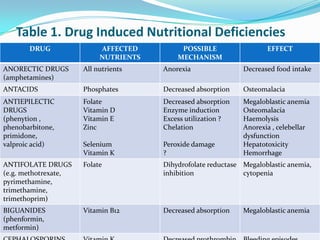
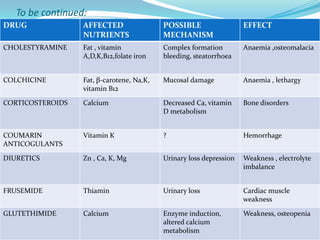
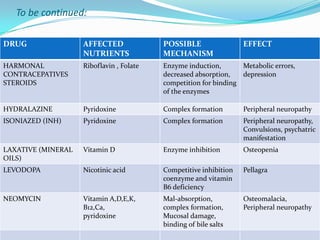
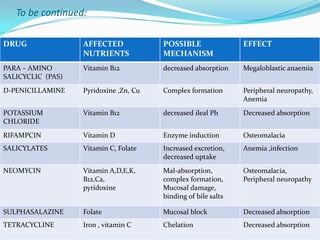
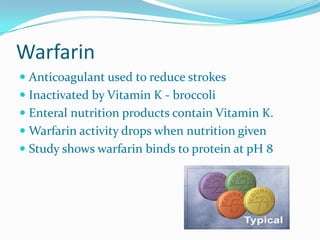
This document discusses food-drug interactions, including how foods can impact drug absorption, distribution, metabolism, and excretion. It provides examples of how foods and nutrients can interact with medications to decrease or increase their intended effects. Specifically, it outlines how foods can influence the pharmacokinetics of drugs by altering absorption, enzyme activity, and nutrient levels in ways that either enhance or reduce drug efficacy and safety.