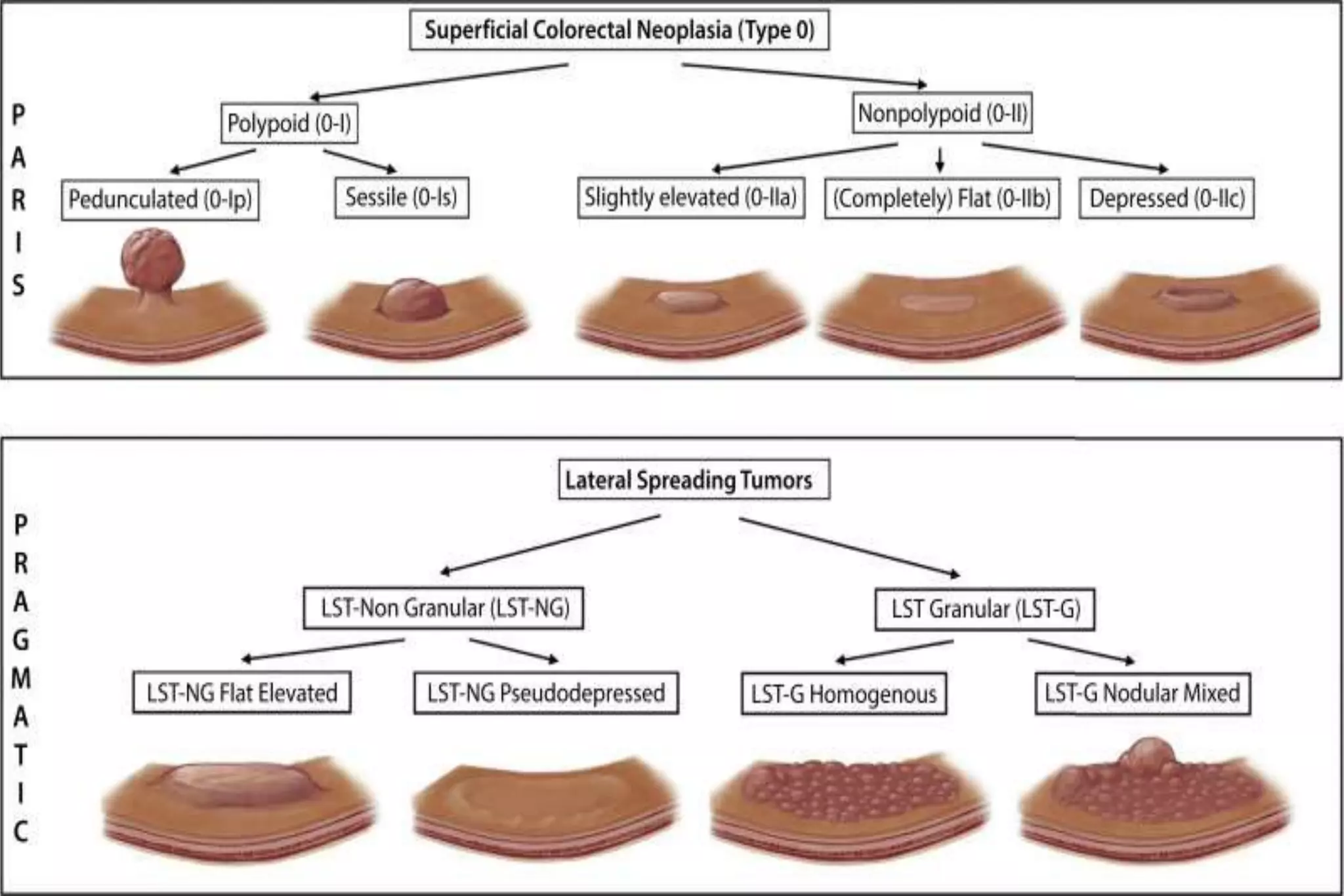
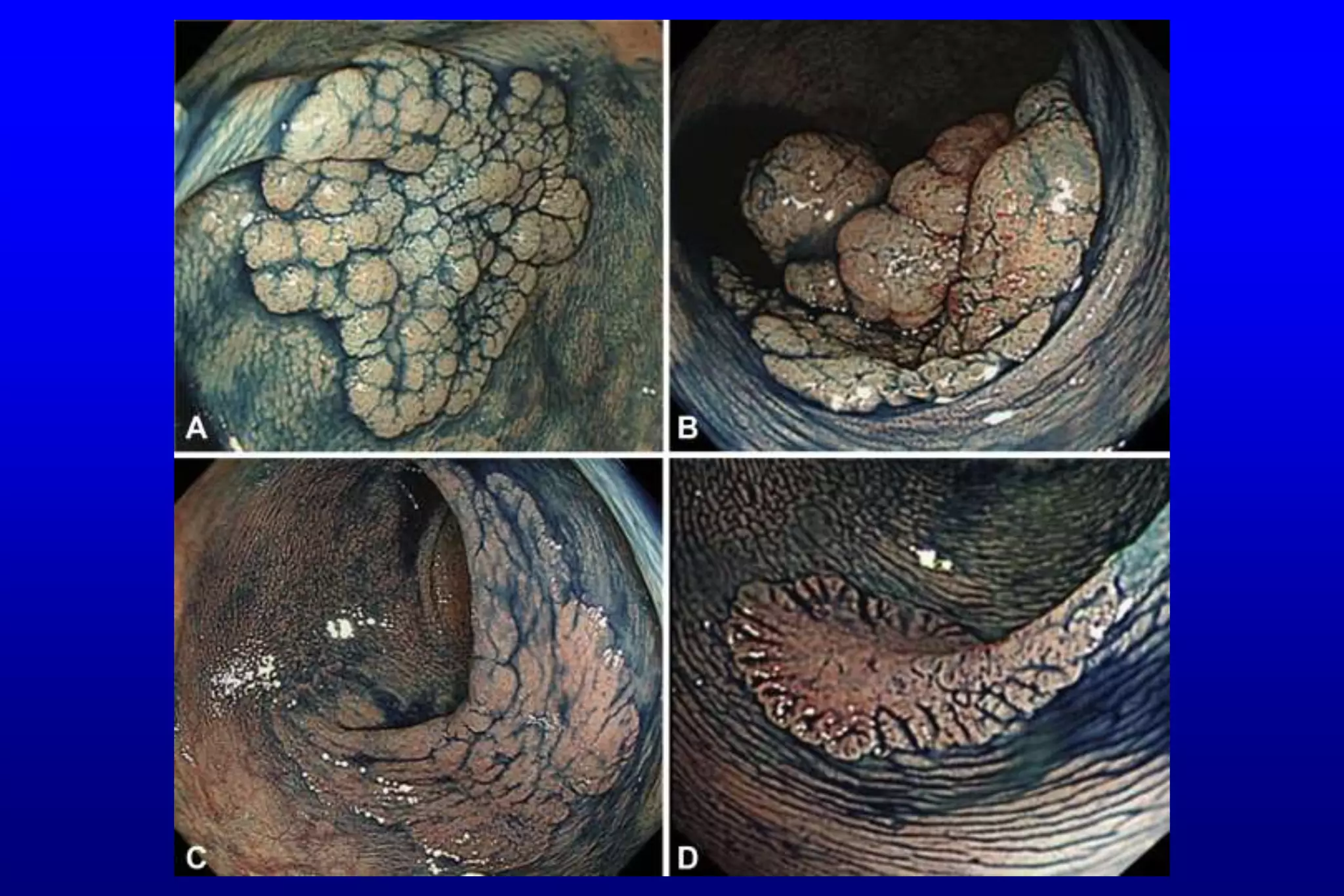
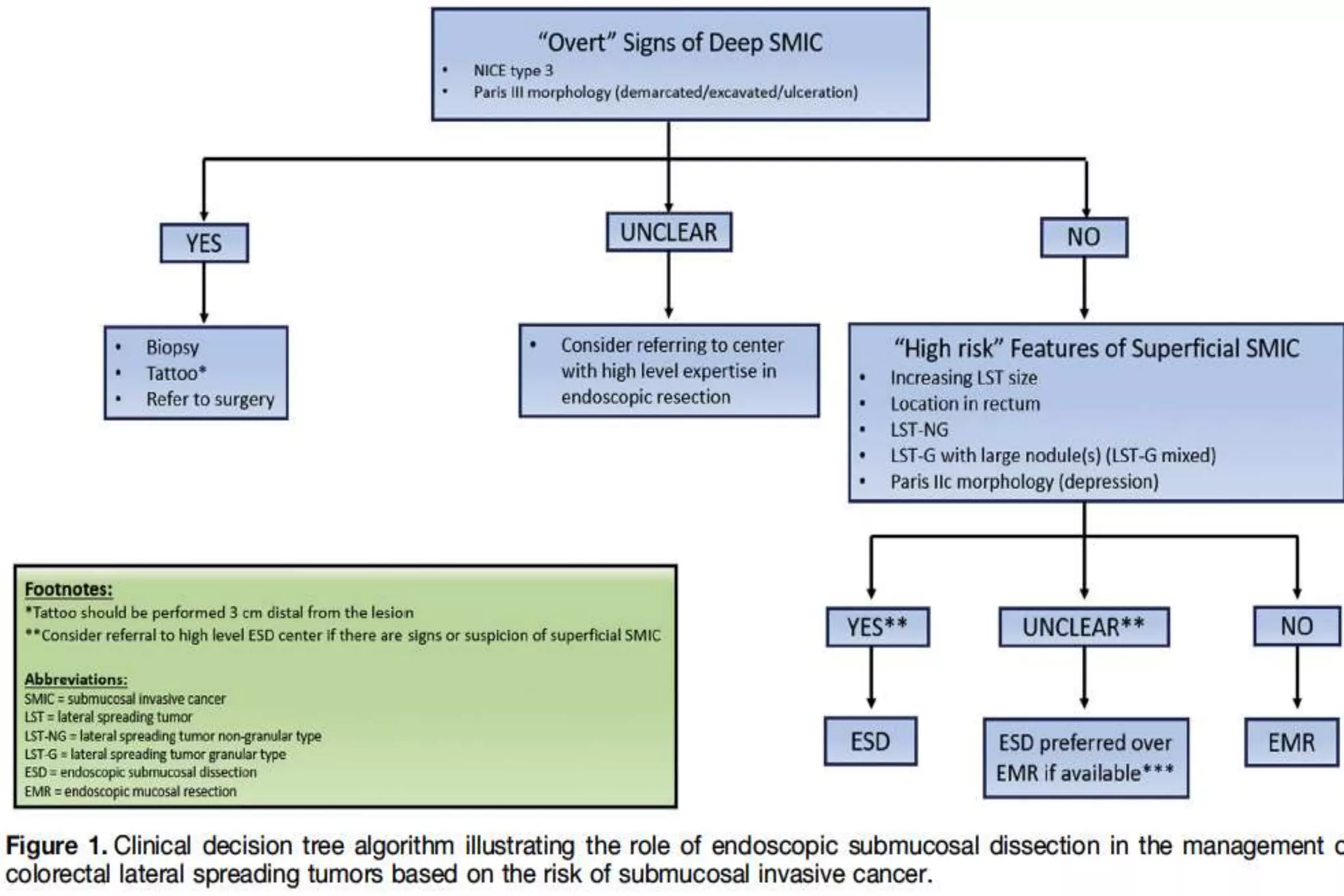
This document discusses the treatment of large sessile colon polyps (LSTs) and the challenges of differentiating between benign and cancerous lesions. It notes that endoscopic mucosal resection (EMR) is usually used but has limitations, while endoscopic submucosal dissection (ESD) enables complete removal and better histological assessment. ESD may avoid unnecessary surgery for lesions with superficial submucosal cancer invasion that can be cured endoscopically. The document reviews different classification systems to predict cancer risk but notes limitations. It advocates that ESD skills and adoption continue improving to help incorporate it more into clinical practice for treating difficult colon polyps.