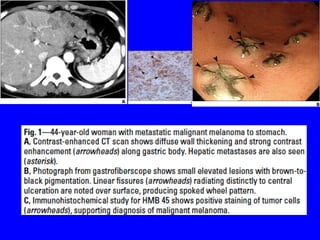
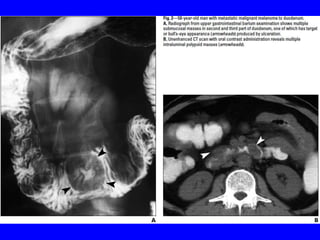
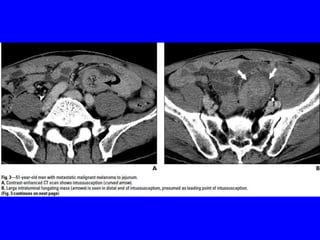
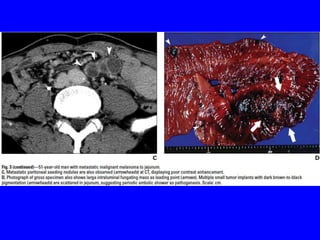
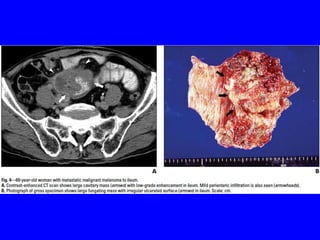
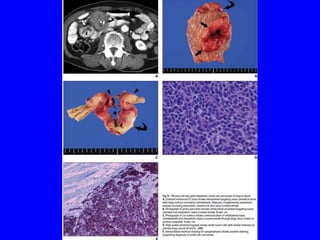
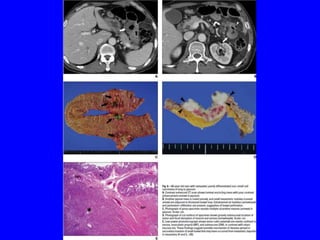
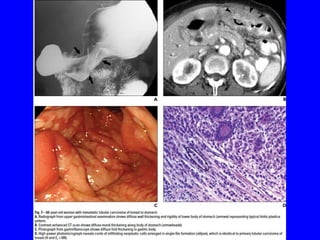
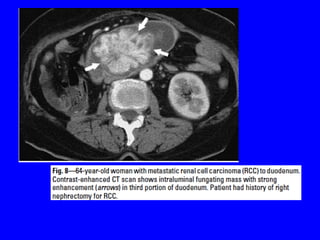
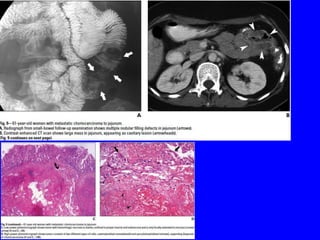
This document discusses gastrointestinal (GI) tract metastases from various primary cancers. It notes that melanoma, lung cancer, and breast cancer most commonly metastasize to the GI tract. The presentation of GI metastases can be variable and nonspecific, with gastrointestinal bleeding or abdominal pain being most common. Endoscopically, metastases may appear as solitary or multiple nodules, ulcers, or subepithelial masses. Diagnosis can be difficult due to the often prolonged time between primary tumor and metastasis, as well as benign-appearing lesions that can mimic primary GI cancers. Advanced imaging like CT and EUS-guided biopsy help confirm diagnoses. Familiarity with metastatic patterns from common primary cancers aids in detection and prevents misdiag