- Galactose is obtained through the diet primarily from lactose in milk and is metabolized mainly in the liver. It is converted to glucose through a series of enzymatic reactions involving galactokinase, galactose-1-phosphate uridylyltransferase, and UDP-glucose 4-epimerase.
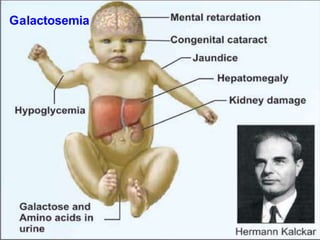
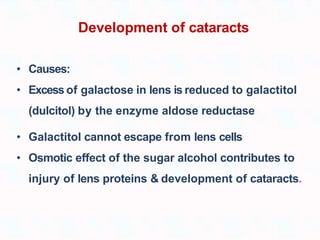
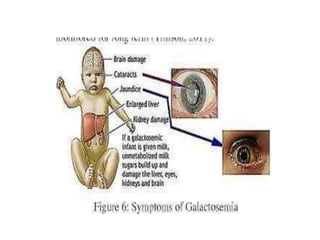
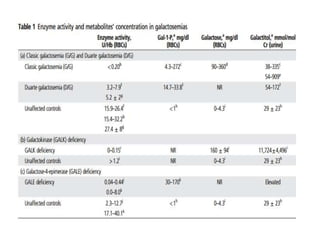
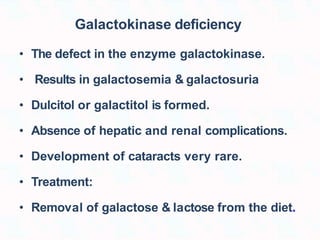
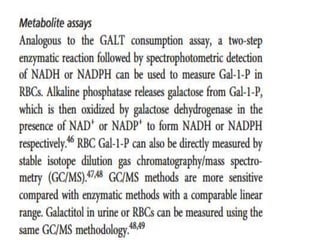
- Deficiencies of galactokinase or galactose-1-phosphate uridylyltransferase can cause galactosemia, leading to an accumulation of galactose and its metabolites in tissues and symptoms including liver damage, cataracts, and intellectual disability.
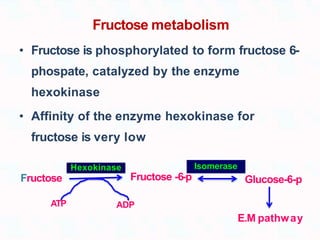
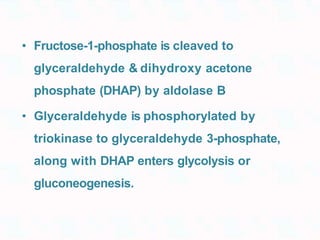
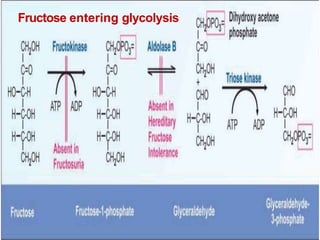
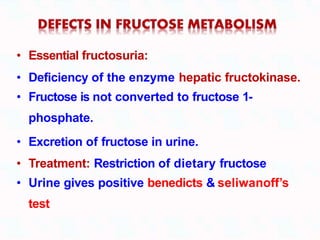
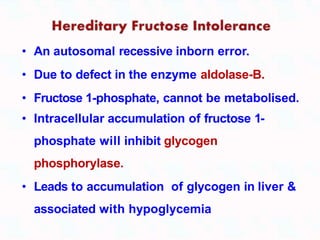
- Fructose obtained through the diet is converted to glucose mainly in the liver