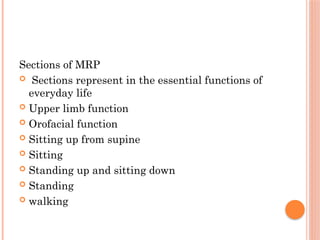
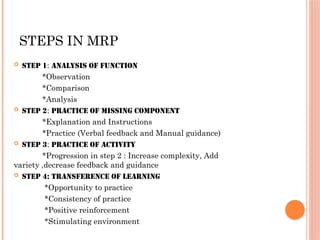
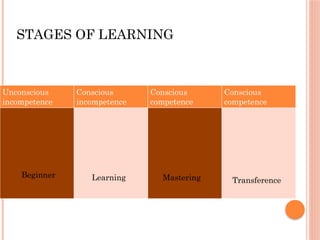
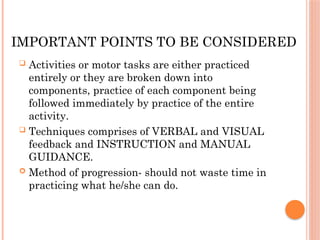
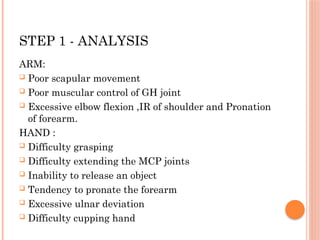
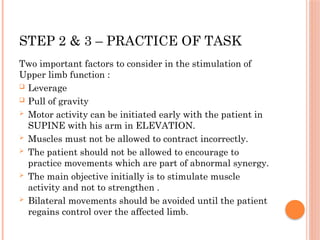
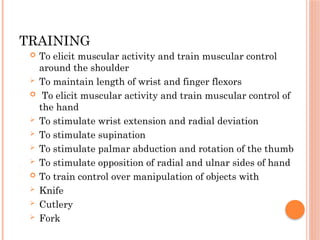
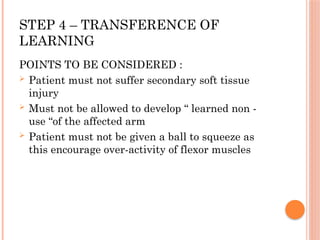
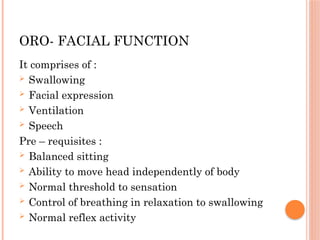
The Motor Relearning Programme (MRP) is a rehabilitation strategy aimed at recovering motor functions after central nervous system injuries through task-oriented activities that focus on eliminating unnecessary muscle activity, providing feedback, and allowing extensive practice. The MRP includes methods for retraining upper limb and oro-facial functions and emphasizes the importance of patient engagement and positive reinforcement in a conducive environment. The document outlines specific practice steps, essential components of movement, techniques for training control, and recommendations for optimizing rehabilitation outcomes.