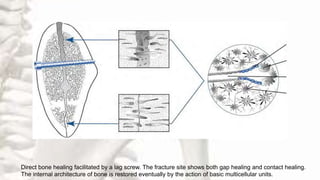
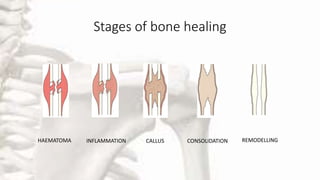
Bone healing is a complex process that occurs in multiple stages to restore injured bone. It involves inflammation, cell proliferation, callus formation, consolidation, and remodeling. There are two main types: healing by direct union, which occurs when fracture ends are close together; and healing by callus formation, which involves five stages over several months. Many local and systemic factors can influence bone healing, and treatment aims to properly position fragments, stabilize fractures, and use grafting when needed. Complications include malunion, delayed healing, non-union, and infection.