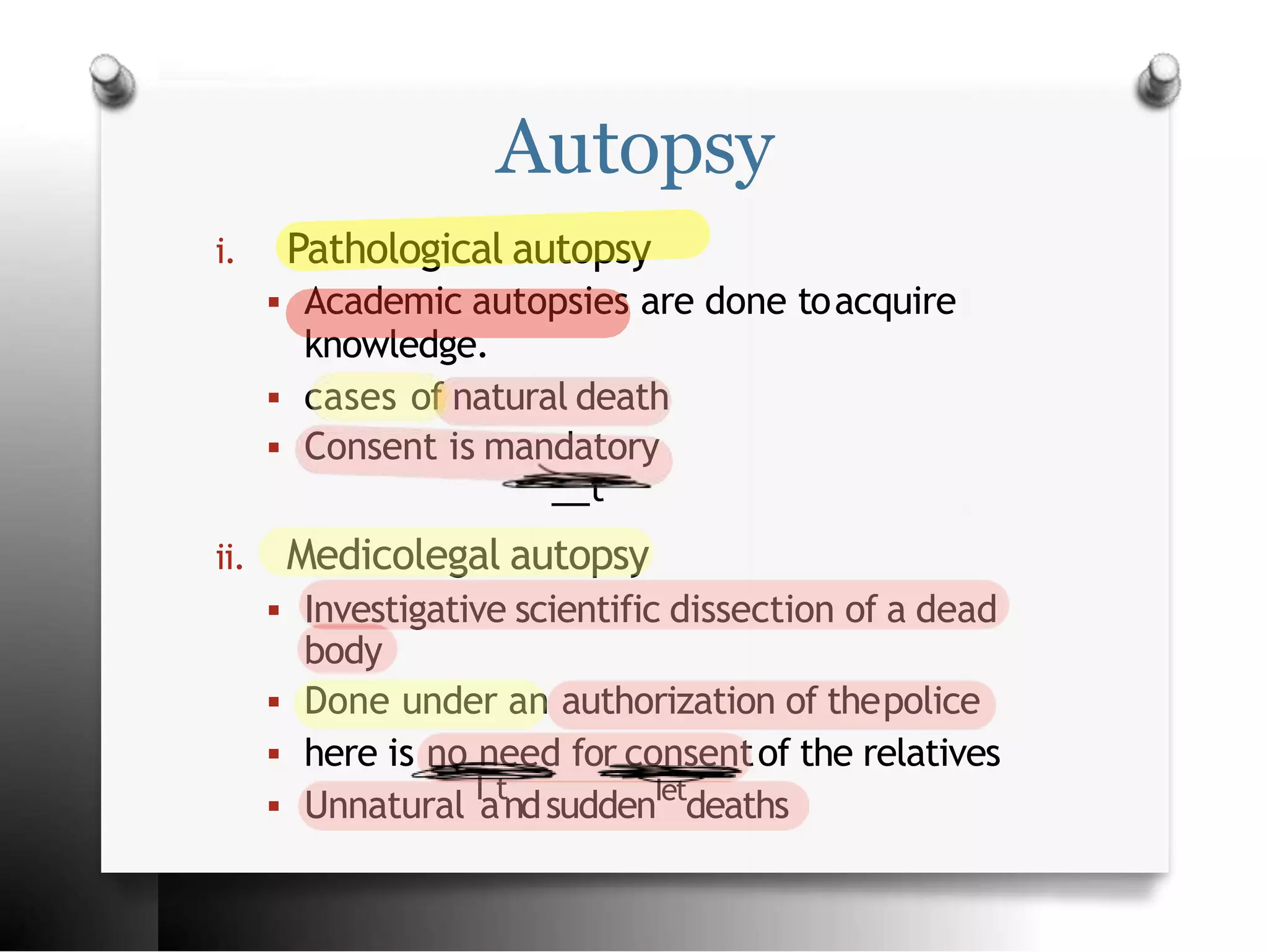
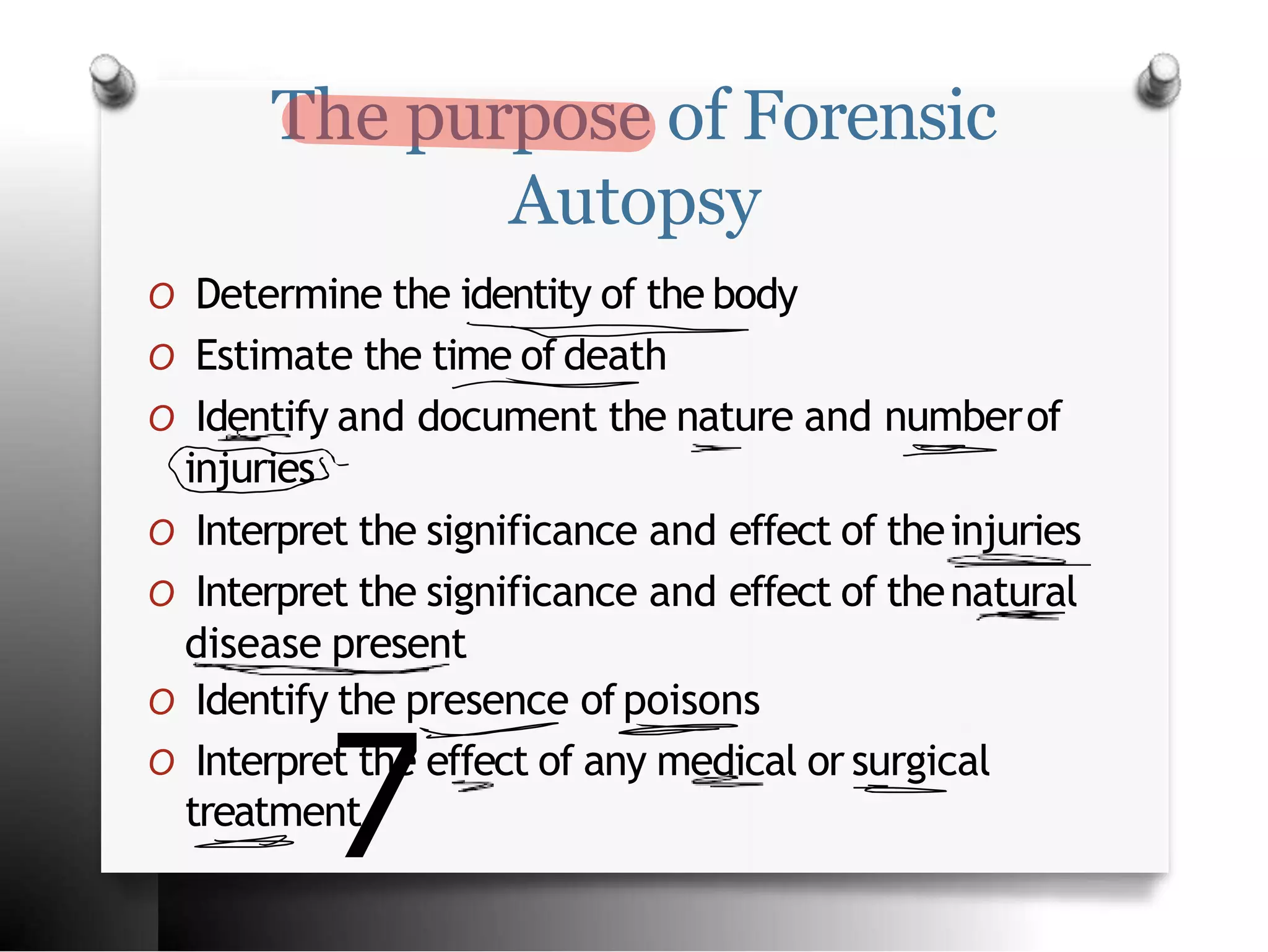
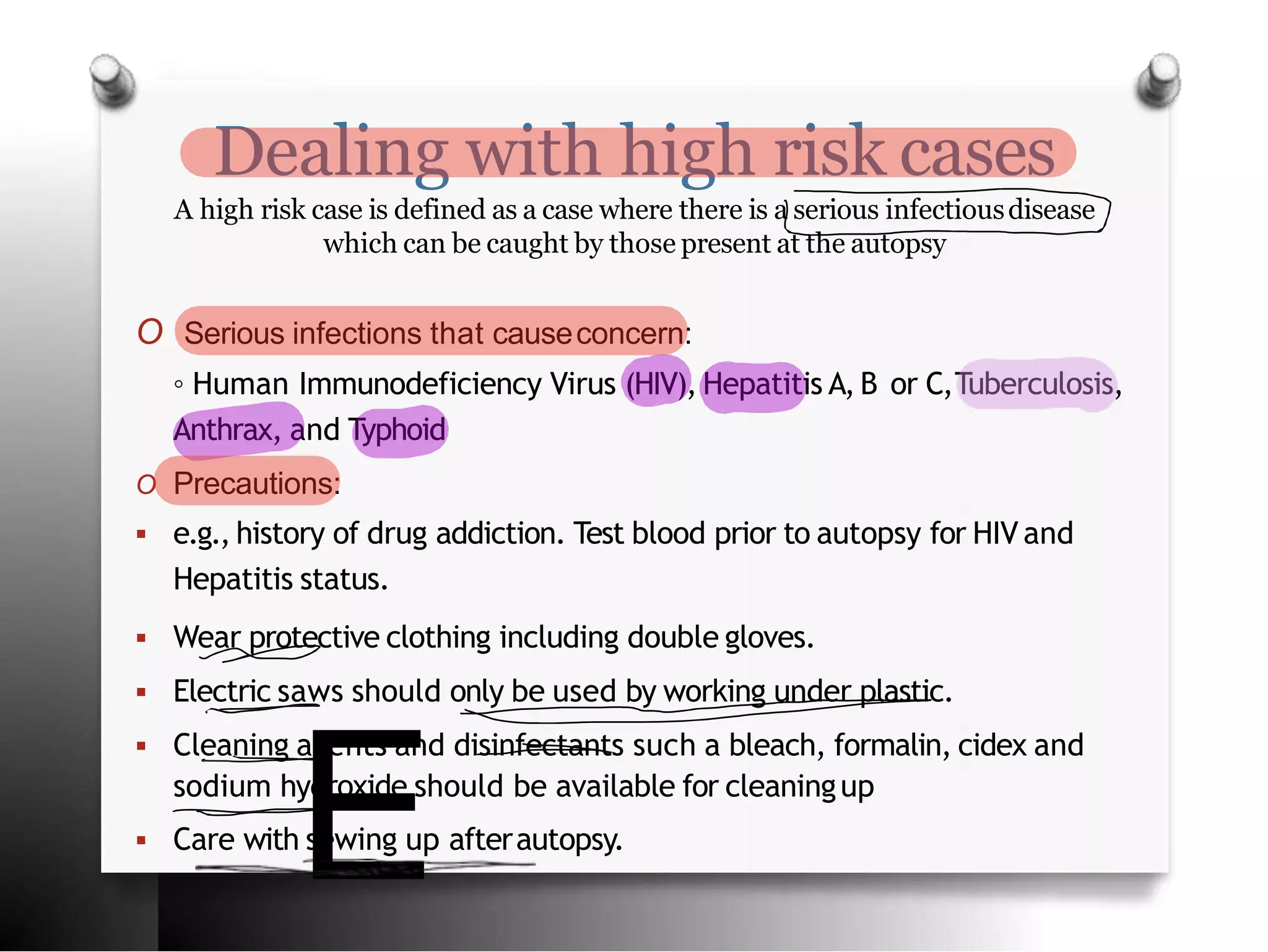
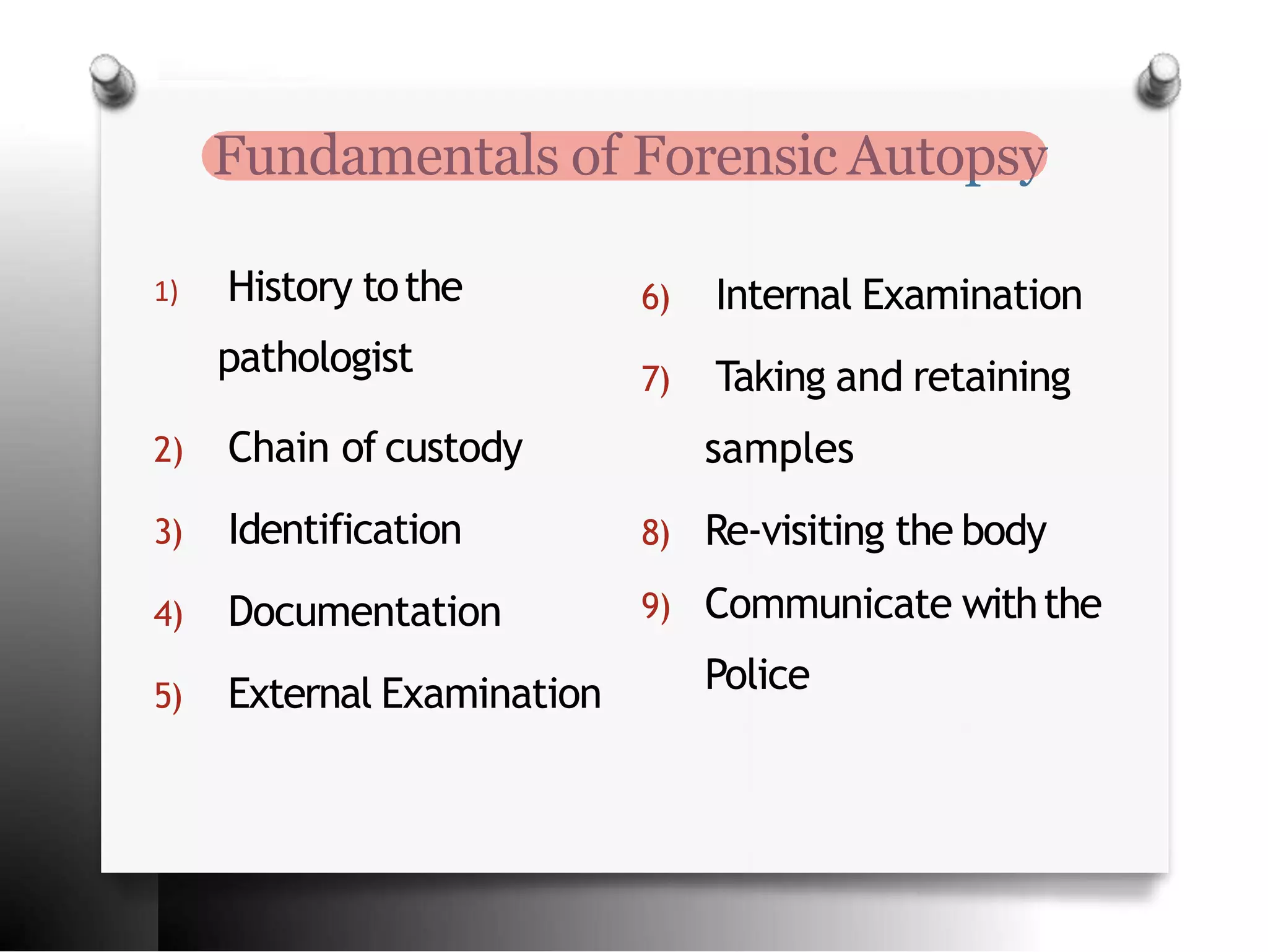
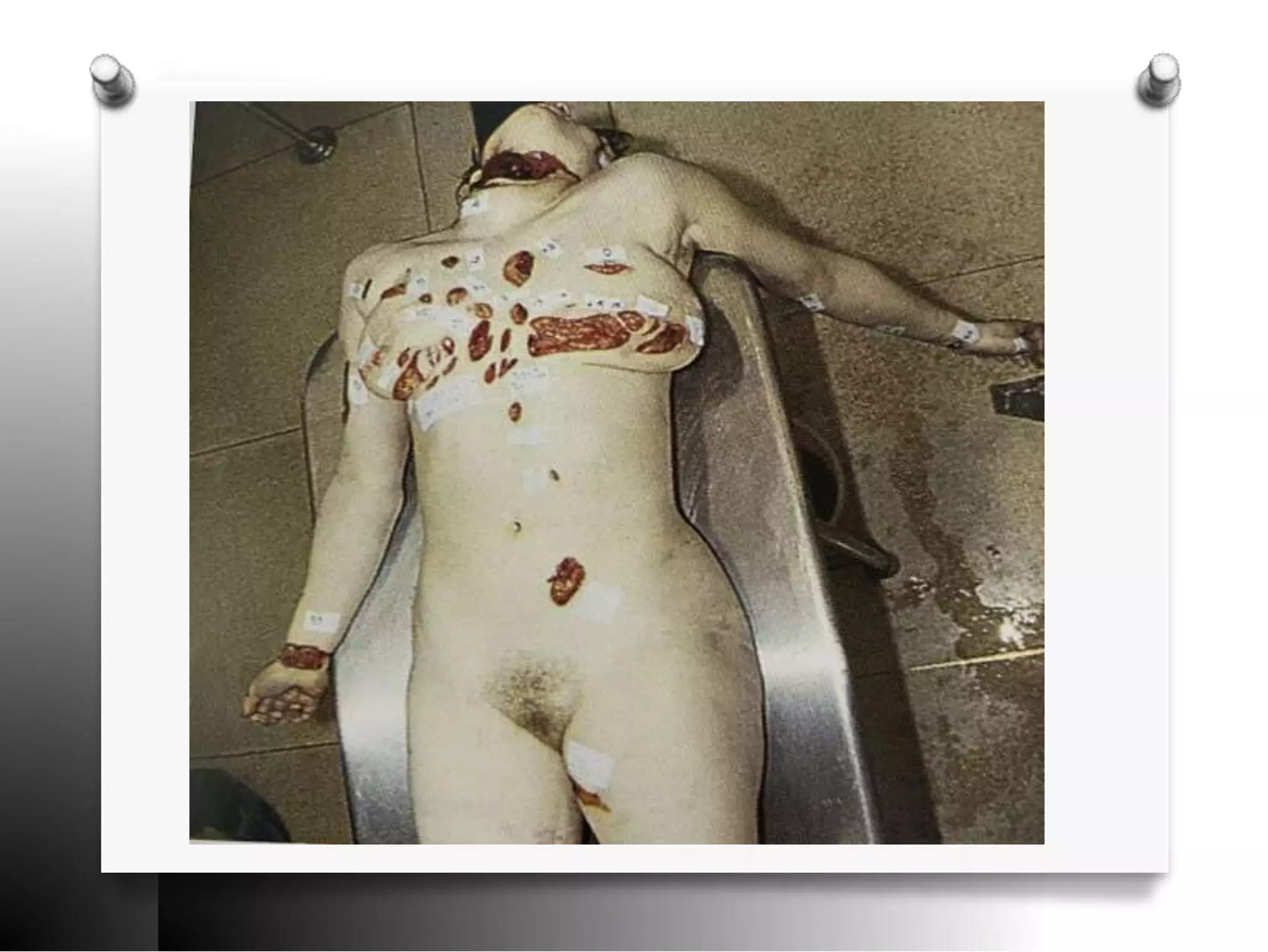
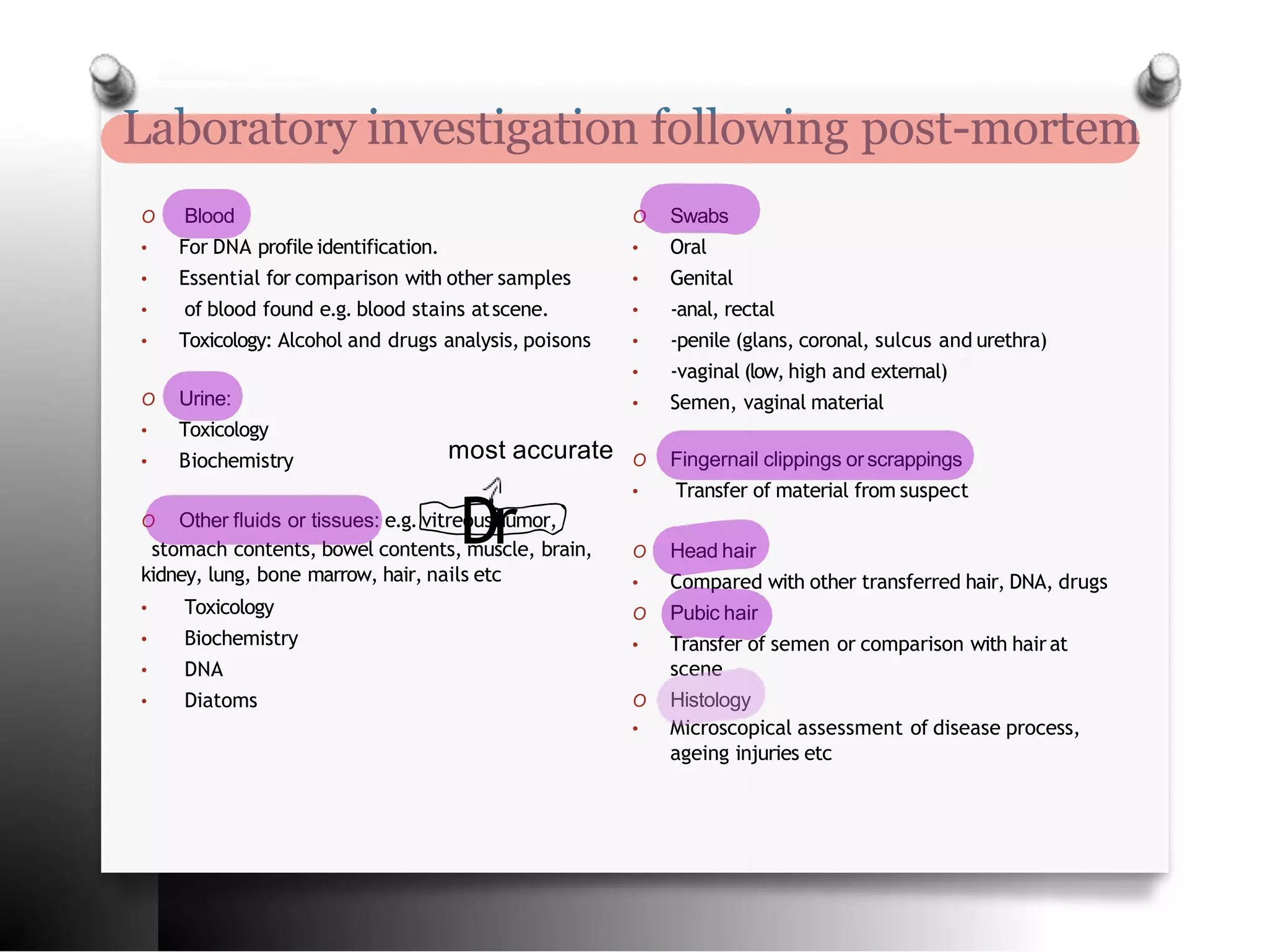
The document discusses the process and objectives of a forensic autopsy. It explains that a forensic autopsy aims to determine the identity of the deceased, estimate the time of death, identify injuries and their significance, and determine the cause of death. The key aspects of a forensic autopsy include external and internal examination of the body, documentation of evidence, laboratory investigation of samples, and preparation of a report detailing the findings and cause of death. Precautions must be taken with high-risk infectious cases. The ultimate goals are to determine the medical cause and manner of death, which may be natural, accidental, suicidal or homicidal.