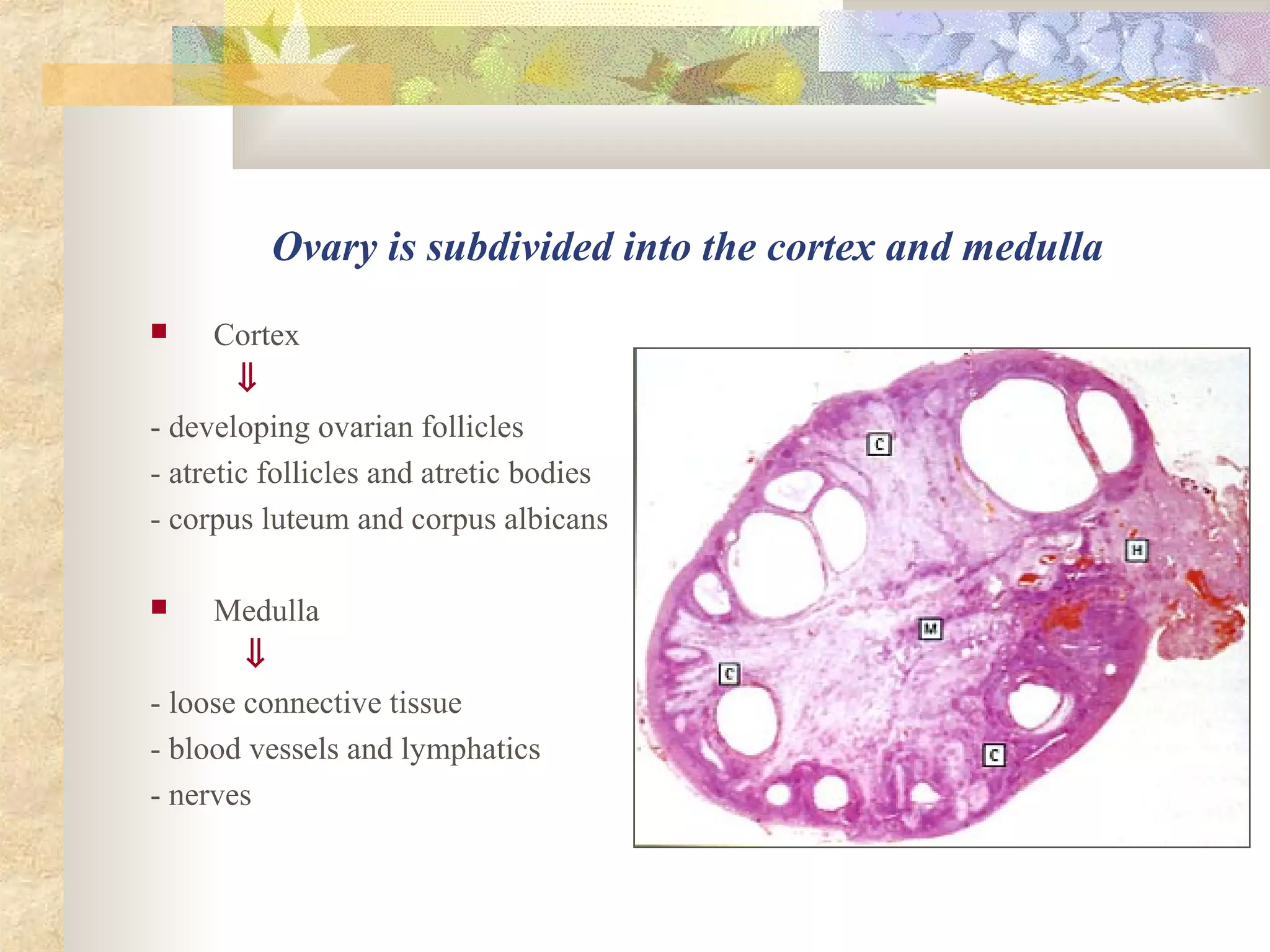
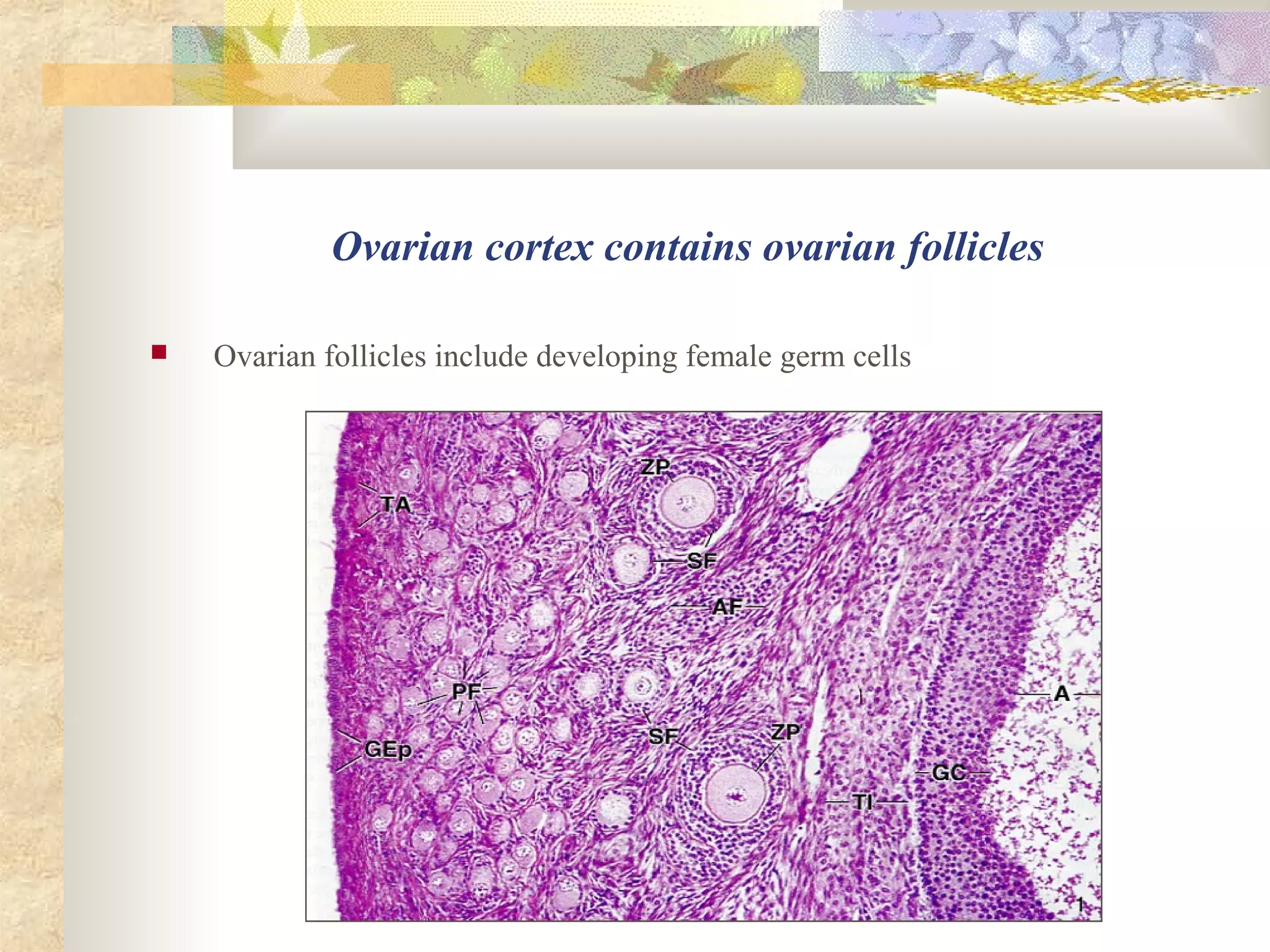
The document summarizes key aspects of the female reproductive system, including the ovaries, oviducts, uterus, and vagina. It describes the structure and functions of the ovaries, including oogenesis and folliculogenesis. It explains how follicles develop from primordial to tertiary stages and the roles of hormones like FSH, LH, and estrogens in follicle development and ovulation. After ovulation, it describes corpus luteum formation and the roles of the corpus luteum in pregnancy or menstruation. It also briefly discusses atresia, the degeneration of ovarian follicles.