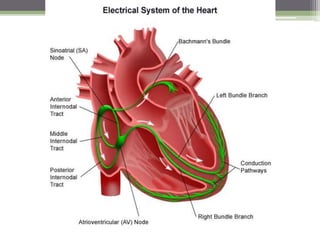
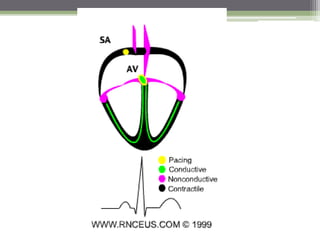
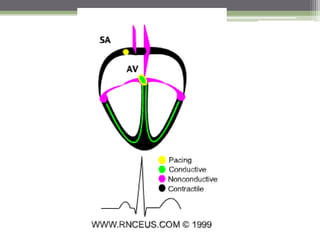
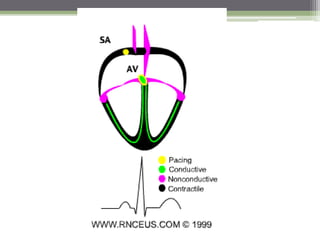
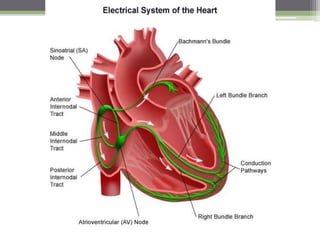
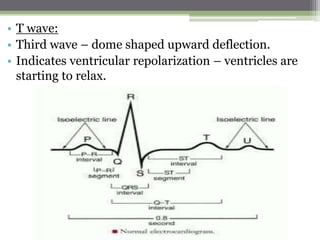
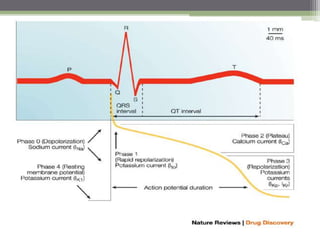
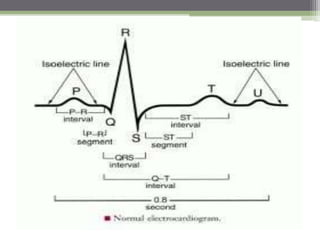
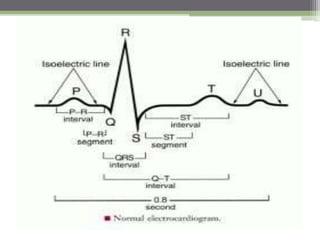
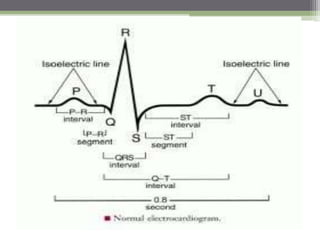
The document summarizes the cardiac conduction system and electrocardiogram (ECG). It describes how the conduction system initiates and propagates electrical signals throughout the heart to coordinate contractions. Specialized pacemaker cells in the sinoatrial node initiate signals that spread through atria and ventricles via pathways like the atrioventricular node and bundle of His. This electrical activity generates currents detectable by ECG, which can provide information on conduction abnormalities and heart health.