X-ray quantity and intensity are affected by several factors:
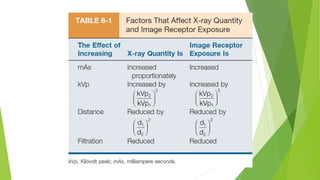
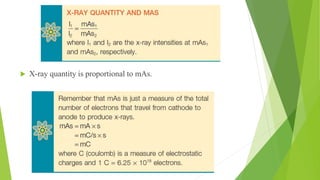
1) Milliampere seconds (mAs) - X-ray quantity is directly proportional to mAs, so doubling mAs doubles the number of x-rays.
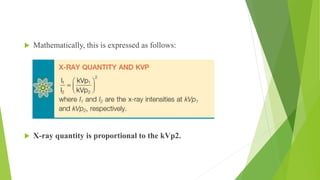
2) Kilovolt peak (kVp) - Doubling kVp quadruples x-ray intensity as it varies with the square of kVp. Increasing kVp by 15% requires reducing mAs by half to maintain constant exposure.
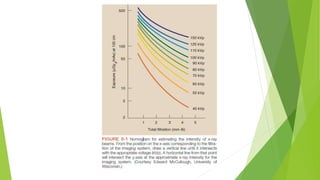
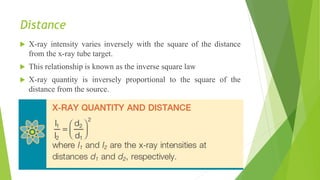
3) Distance - X-ray intensity varies inversely with the square of the distance from the source, following the inverse square law. Doubling the source-image distance requires quadrupling m

![X-ray Intensity
The intensity of the x-ray beam of an x-ray imaging system is measured
in milligray in air (mGya) [formerly milliroentgen (mR)] and is called
the x-ray quantity.
Another term, radiation exposure, is also often used. All have the same
meaning, and all are measured in mGya (mR).
The mGya (mR) is a measure of the number of ion pairs produced in air
by a quantity of x-rays.](https://image.slidesharecdn.com/factoraffectingthequantityofxray-230810183303-45a7b4b3/85/Factor-affecting-the-quantity-of-Xray-pptx-4-320.jpg)