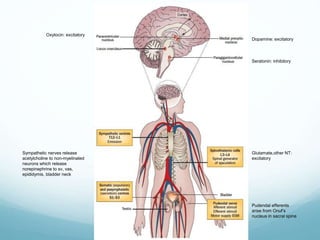
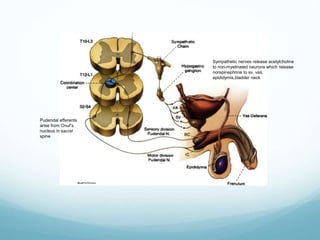
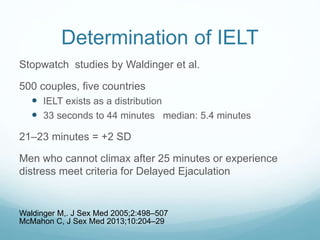
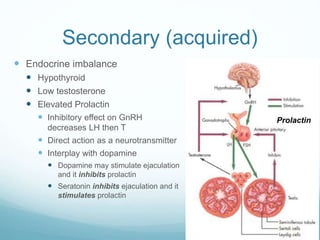
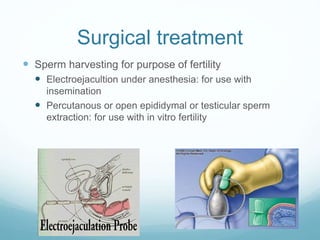
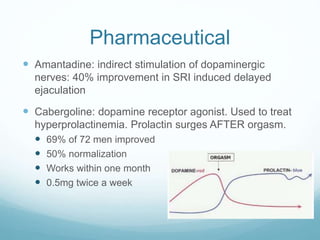
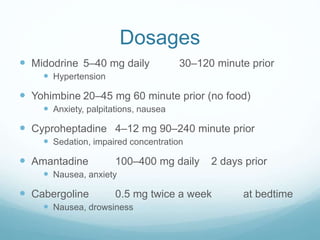
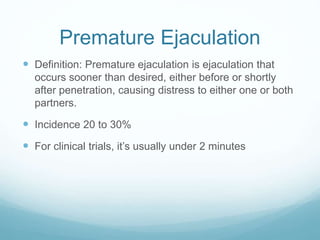
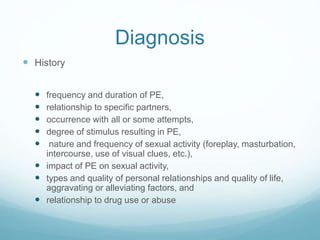
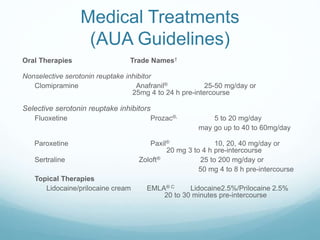
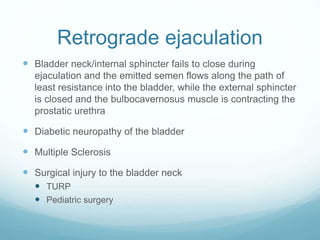
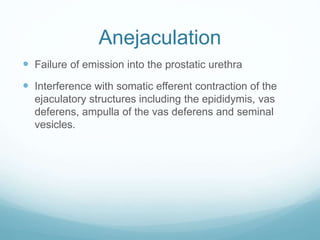
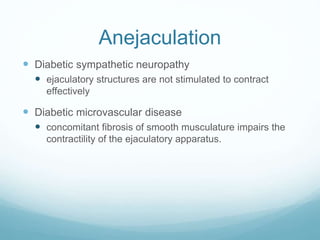
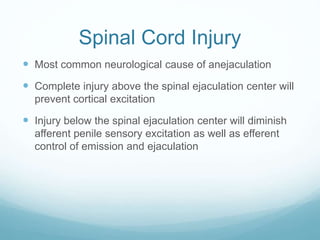
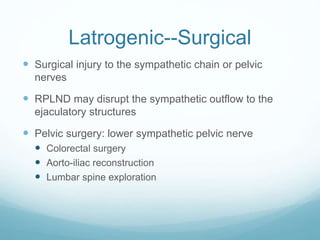
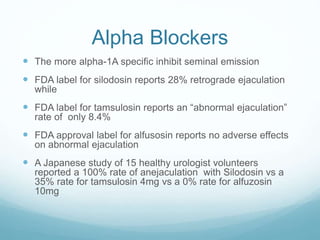
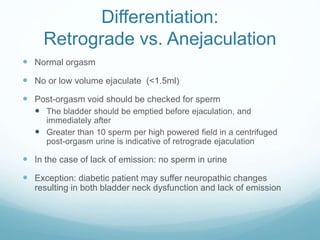
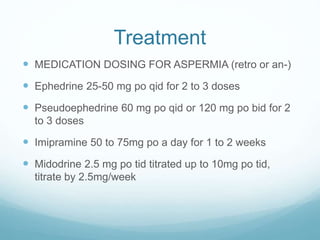
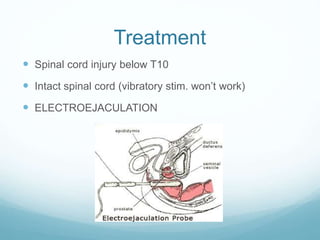
The document discusses various disorders of ejaculation, including delayed ejaculation, premature ejaculation, retrograde ejaculation, and anejaculation, highlighting their medical, psychological, and surgical causes. It also covers the role of neurotransmitters and hormones in ejaculatory function, diagnostic approaches, and treatment options, such as pharmacological therapies and psychosexual counseling. Each disorder is elaborated upon, with insights into incidence rates, diagnosis criteria, and specific medications or interventions used for treatment.