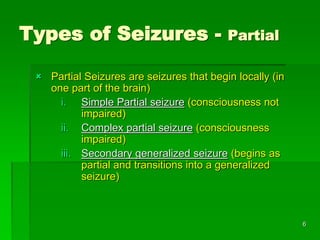
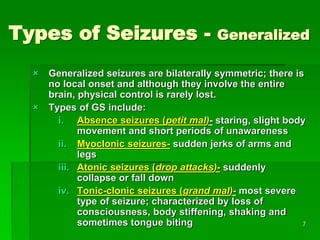
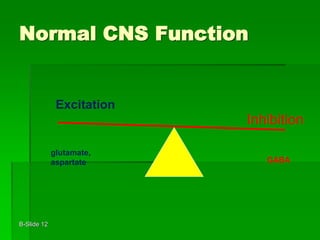
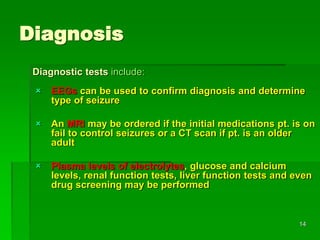
This document provides an overview of epilepsy, including definitions, types of seizures, causes, diagnosis, and treatment options. It defines epilepsy as a chronic neurological disorder characterized by recurrent seizures. Seizures occur due to abnormal electrical activity in the brain and can be classified as either partial or generalized depending on where they originate. Causes of epilepsy include genetic factors, brain injury, infection, and tumors. Diagnosis involves EEG, MRI or CT scans. Treatment primarily consists of anti-epileptic medications, though surgery may be an option for localized seizures. The majority of epilepsy patients can achieve seizure control through medication.