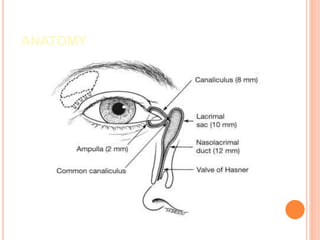
Dacryocystorhinostomy (DCR) surgery is performed to restore tear drainage from the lacrimal sac into the nose when the nasolacrimal duct is blocked. There are several types but external DCR involves making incisions in the skin and nasal mucosa to create flaps and suturing them together to bypass the blockage. Preoperative testing and nasal packing is done prior to general anesthesia. The procedure exposes and removes bone between the lacrimal sac and nose to join the spaces. Silastic tubes may be placed short term and patients are monitored after for potential early, intermediate or late complications like infection, scarring or restenosis.