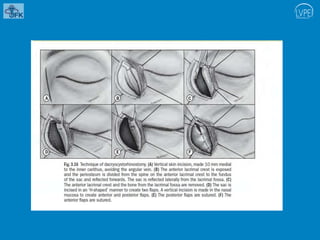
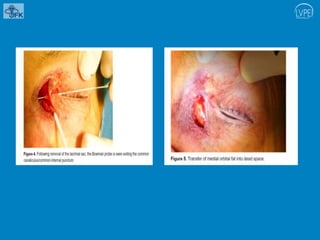
The document discusses dacrocystitis, an infection of the lacrimal sac often caused by obstruction of the nasolacrimal duct, with clinical presentations including pain, swelling, and potential complications like abscess formation. Treatment options range from warm compresses and antibiotics to surgical interventions like dacryocystorhinostomy and dacryocystectomy, depending on the severity and nature of the condition. The document details various surgical techniques, success rates, and potential complications associated with these procedures.