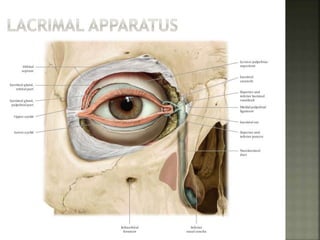
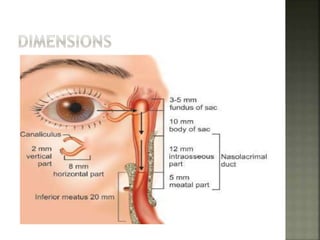
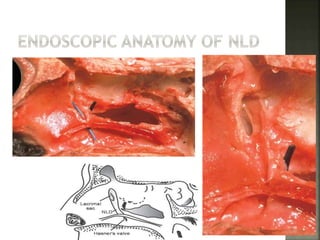
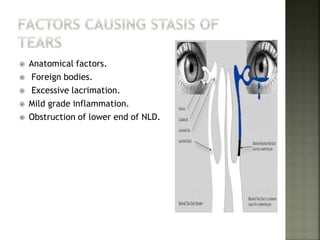
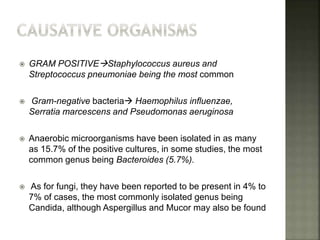
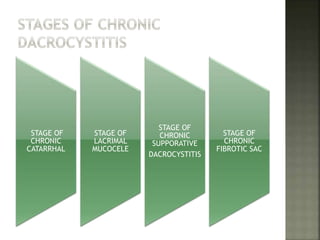
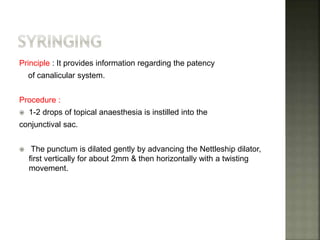
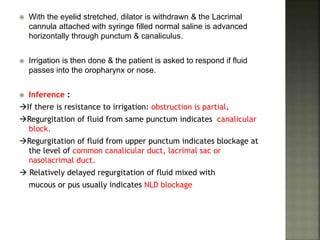
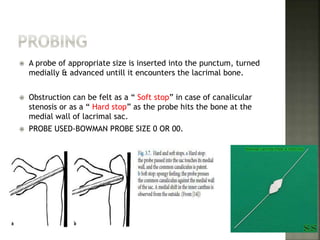
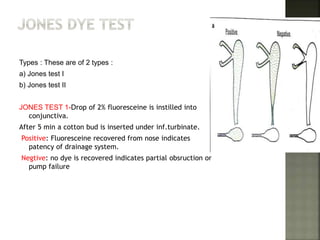
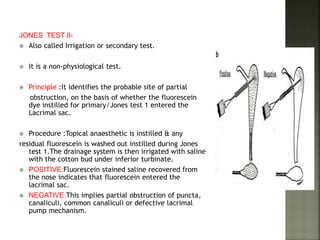
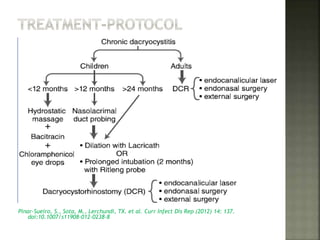
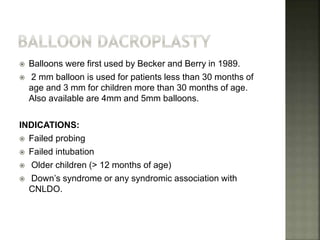
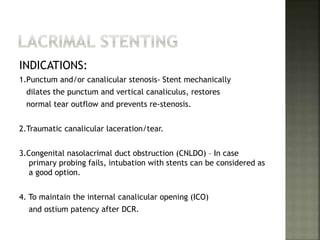
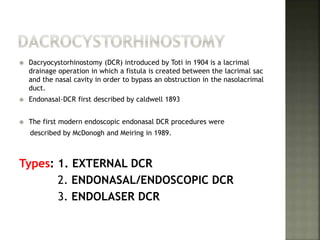
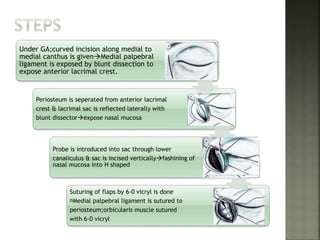
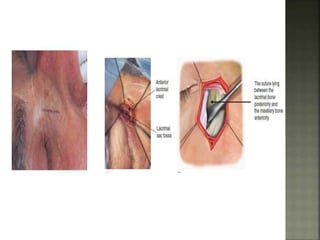
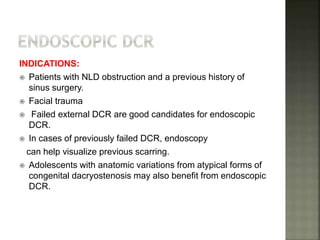
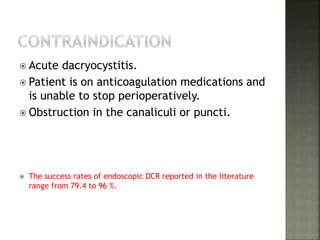
Dacryocystitis is an infection of the lacrimal sac caused by obstruction of the nasolacrimal duct. The main cause is distal obstruction of the nasolacrimal duct, leading to tear retention in the lacrimal sac. Clinical evaluation includes syringing and probing to assess the level of obstruction. Treatment depends on the stage but may include intubation, balloon dacryoplasty, or dacryocystorhinostomy to surgically create a passage from the lacrimal sac to the nasal cavity.