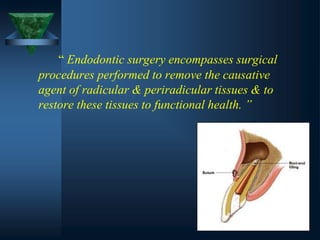
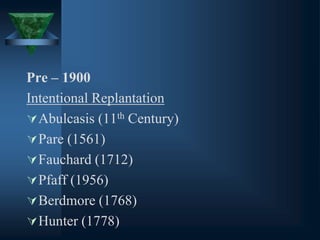
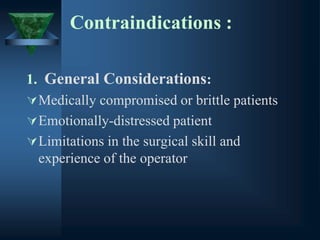
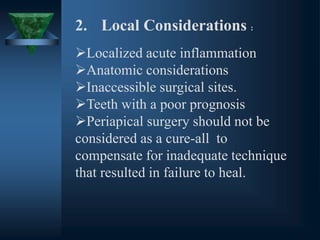
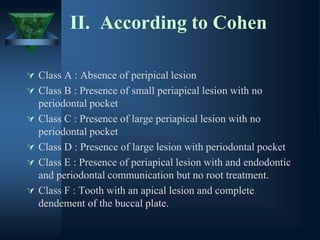
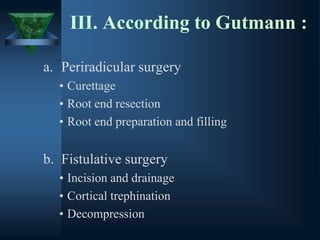
This document provides an overview of endodontic surgery. It begins with an introduction and then discusses the historical perspectives of endodontic surgery. It outlines the objectives, indications, classifications, and various surgical techniques including surgical drainage, periradicular surgery, consent, preoperative evaluation, anesthesia, soft tissue management, hard tissue management, and postoperative patient management. It also discusses recent advances in endodontic microsurgery, corrective surgery, and concludes with references. The document provides essential information on endodontic surgery procedures and considerations.




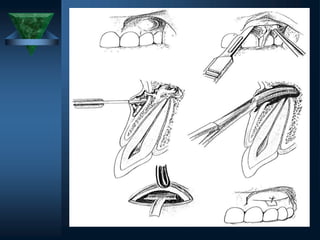




![CLASSIFICATION OF
SURGICAL FLAPS
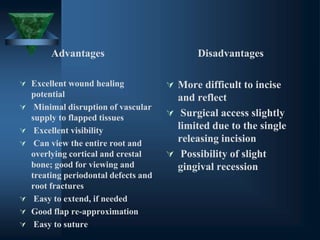
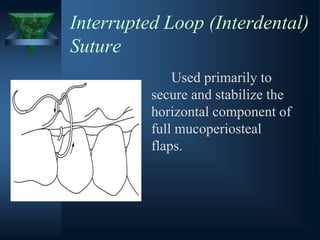
1] Full mucoperiosteal flaps
a) Triangular ( one vertical releasing incision )
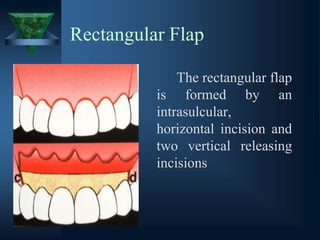
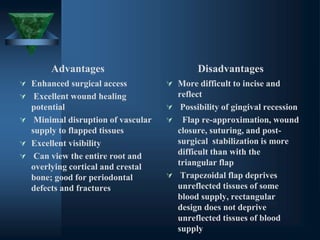
b) Rectangular ( two vertical releasing incision)
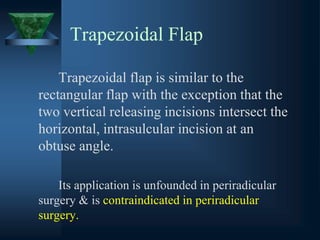
c) Trapezoidal ( broad – based rectangular)
d) Horizontal ( no vertical releasing incision)
2] Limited mucoperiosteal flaps
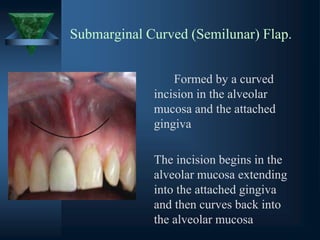
(a) Submarginal curved (semilunar)
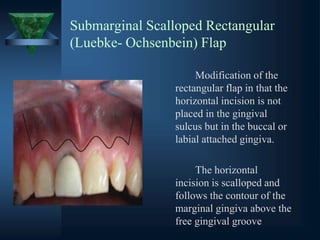
(b) Submarginal scalloped rectangular (Luebke-
Ochsenbein)](https://image.slidesharecdn.com/endodonticsurgery-231010020319-2e3f5219/85/ENDODONTIC-SURGERY-pptx-45-320.jpg)