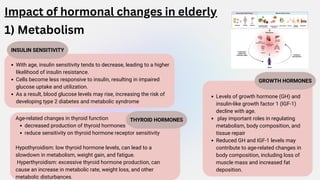
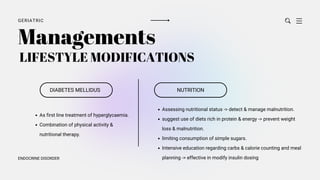
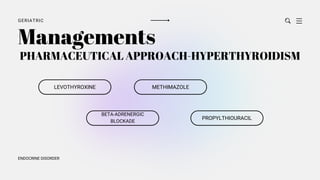
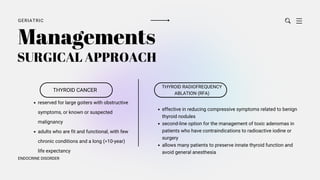
The document discusses the endocrine system and its changes with aging, highlighting alterations in thyroid, growth, and sex hormones, which can lead to various health conditions such as diabetes, hypothyroidism, and hormonal imbalances. It emphasizes the impacts of aging on metabolic processes, muscle mass, and bone density, and outlines management strategies for age-related endocrine disorders, including lifestyle modifications and pharmaceutical approaches. The document concludes by addressing the complexities surrounding hormonal imbalances and their implications for elderly patients.