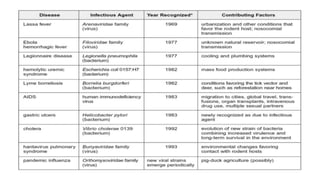
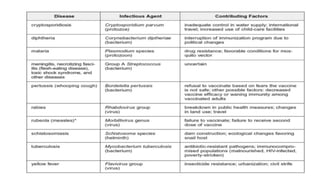
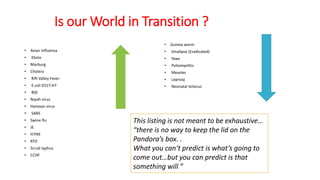
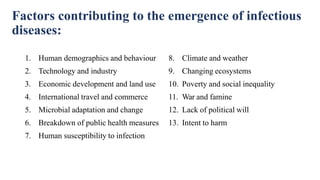
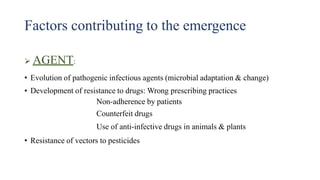
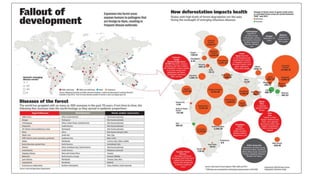
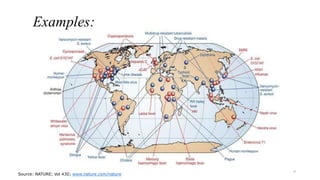
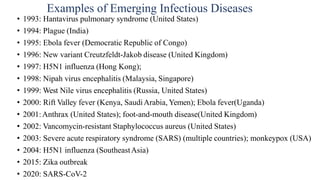
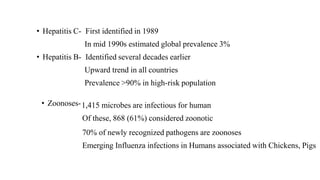
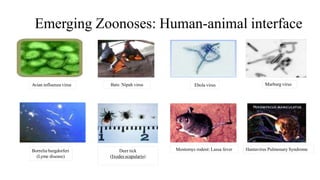
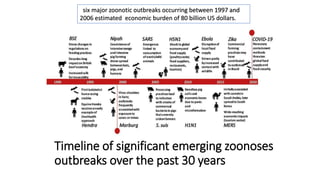
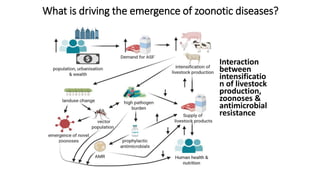
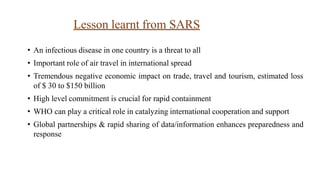
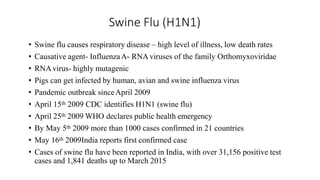
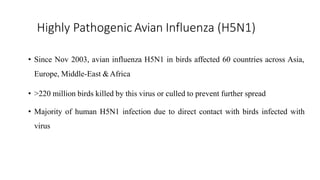
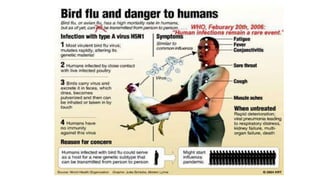
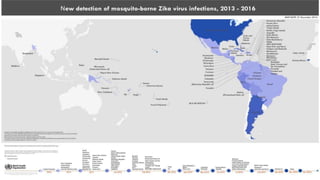
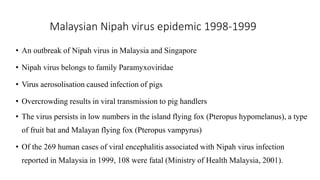
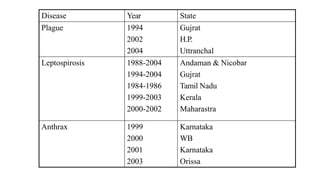
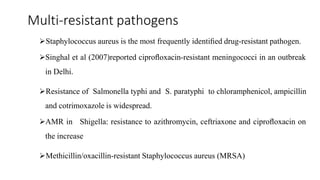
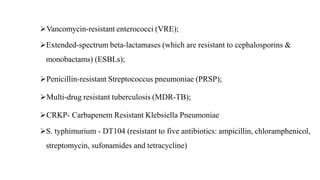
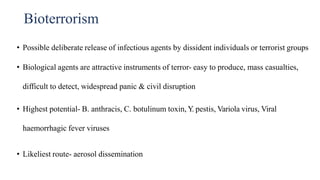
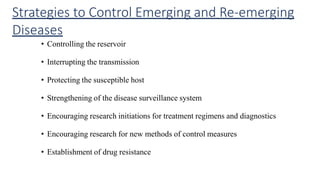
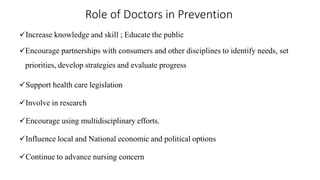
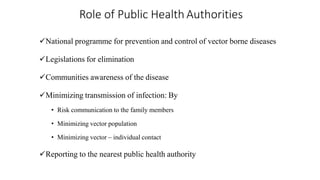
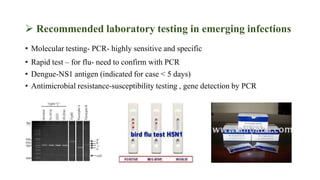
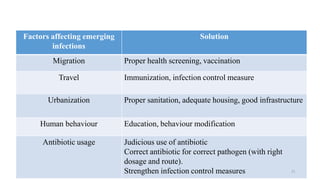
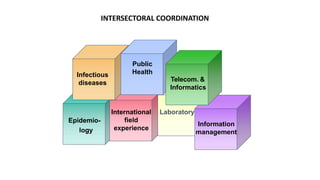
This document discusses emerging and re-emerging infectious diseases. It begins with an introduction that defines emerging diseases as new diseases caused by newly discovered pathogens, while re-emerging diseases are old diseases that were previously controlled but have risen again as health problems. The document then covers the epidemiology of these diseases, including factors contributing to their emergence such as human behavior, travel, and climate change. Examples are provided of diseases like SARS, Ebola, Zika, and antibiotic-resistant pathogens. Strategies for prevention and the roles of doctors, public health authorities, and public health measures are also outlined.