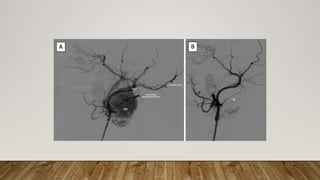
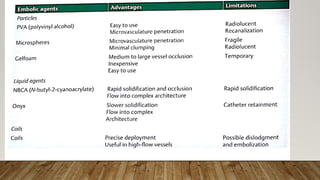
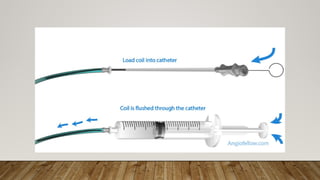
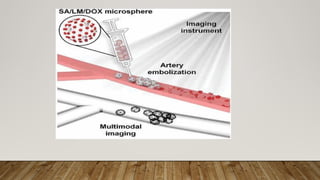
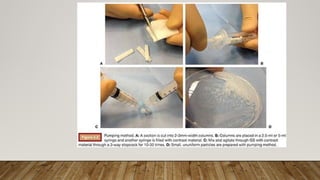
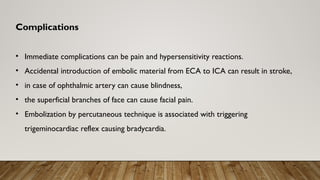
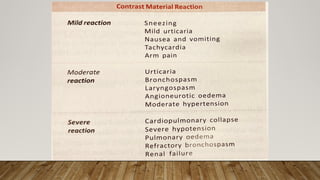
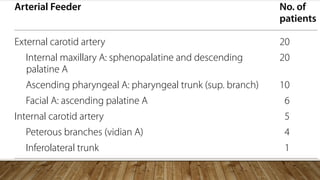
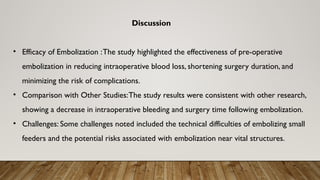
The document discusses the role of preoperative embolization in managing juvenile nasopharyngeal angiofibroma (JNA), highlighting its effectiveness in reducing intraoperative blood loss and improving surgical outcomes. It reviews various techniques, including transarterial and direct percutaneous embolization, with a focus on the successful use of cyanoacrylate glue combined with particulate agents. Overall, the findings support using preoperative embolization as a safe and efficient approach for treating JNA.