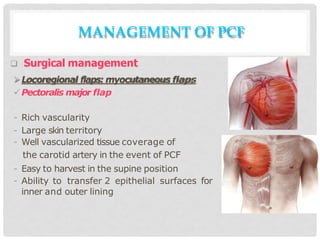
This document discusses the management of pharyngocutaneous fistulas (PCF), which are abnormal connections between the digestive tract and skin in the neck that allow saliva to drain through the skin. It defines PCF and outlines risk factors, symptoms, detection methods, and treatment approaches. Conservative management is attempted first using dressings, nutrition, and antibiotics. Surgical options include primary closure for small fistulas or flap reconstruction using pectoralis major or other regional or free flaps if conservative treatment fails. The goal of management is to prevent PCF through careful surgery and identify comorbidities, detect fistulas early, and employ a multidisciplinary team to treat fistulas using either conservative or surgical methods.