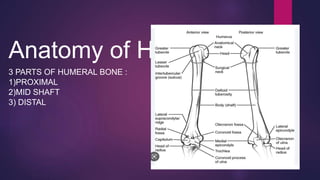
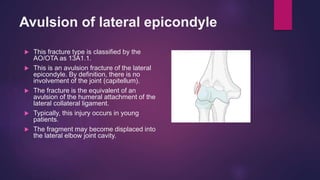
The document discusses fractures of the humerus bone, which has three parts - proximal, mid shaft, and distal. Shaft fractures of the humerus are common in adults from falls and in children. Distal humerus fractures are rare and occur after age 40 from force through the flexed elbow. Treatment depends on the type and location of the fracture, ranging from splinting, casting, and bracing for nondisplaced fractures to open reduction and internal fixation for displaced fractures. Complications can include nerve and blood vessel injuries as well as joint stiffness.