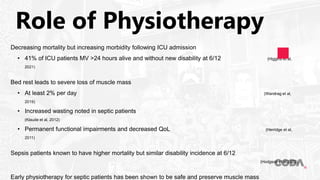
The document discusses the role of physiotherapy in managing sepsis patients in ICU, emphasizing early mobilization and respiratory management to improve outcomes and preserve muscle mass. It highlights the necessity for a multidisciplinary team approach and presents evidence supporting the safety and feasibility of such interventions. Challenges include patient engagement, mobility limitations, and structural barriers within healthcare settings.