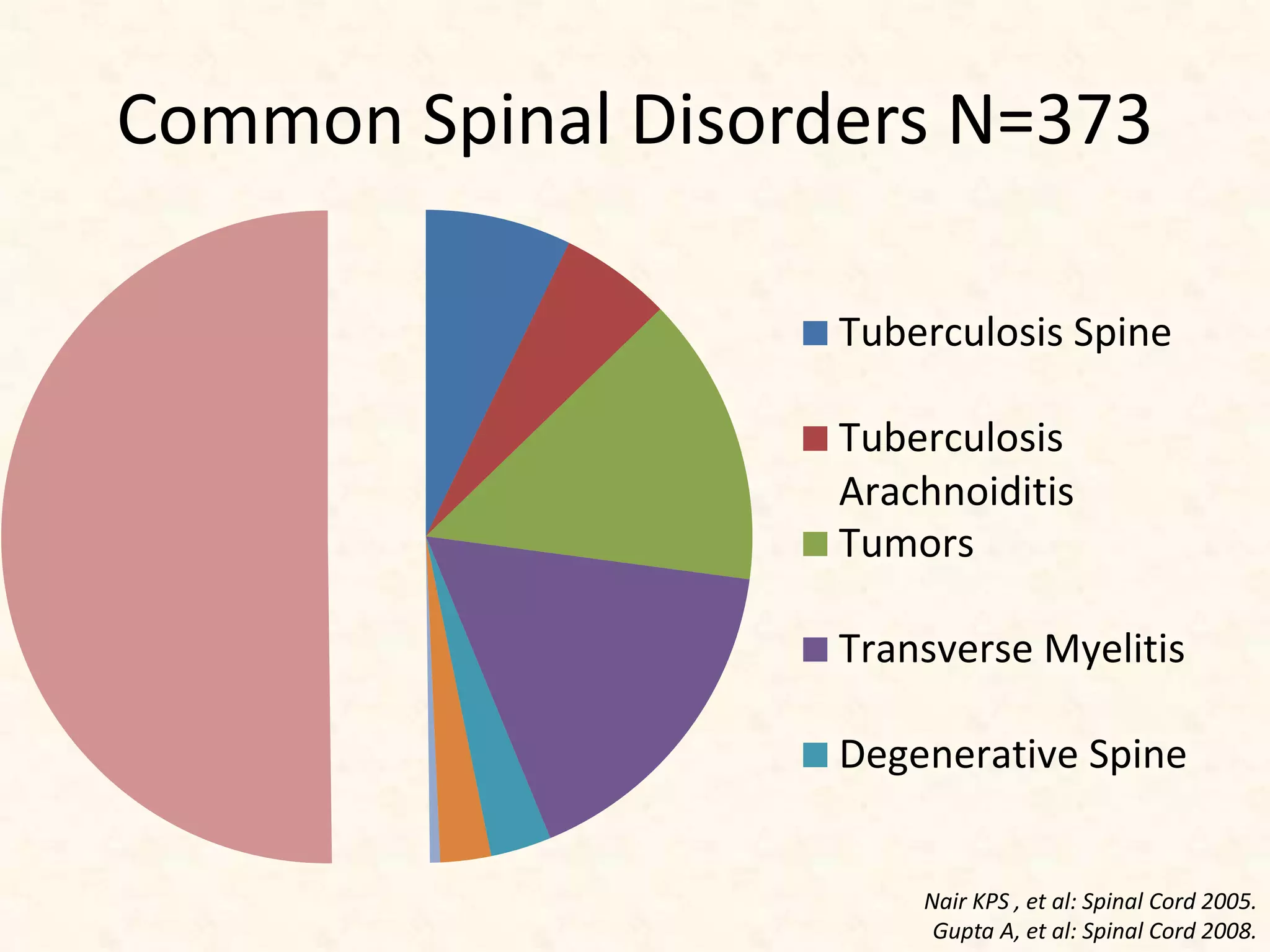
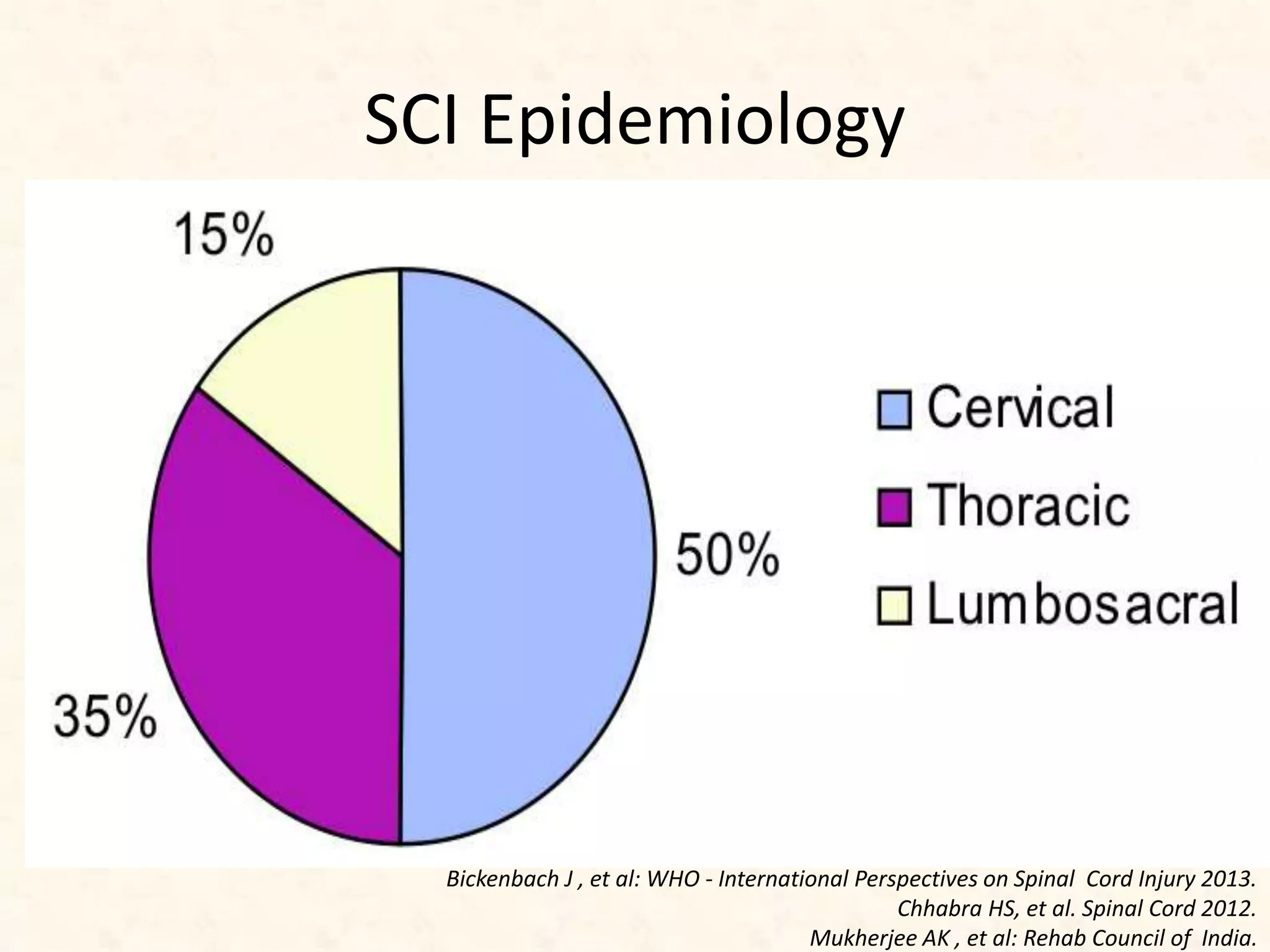
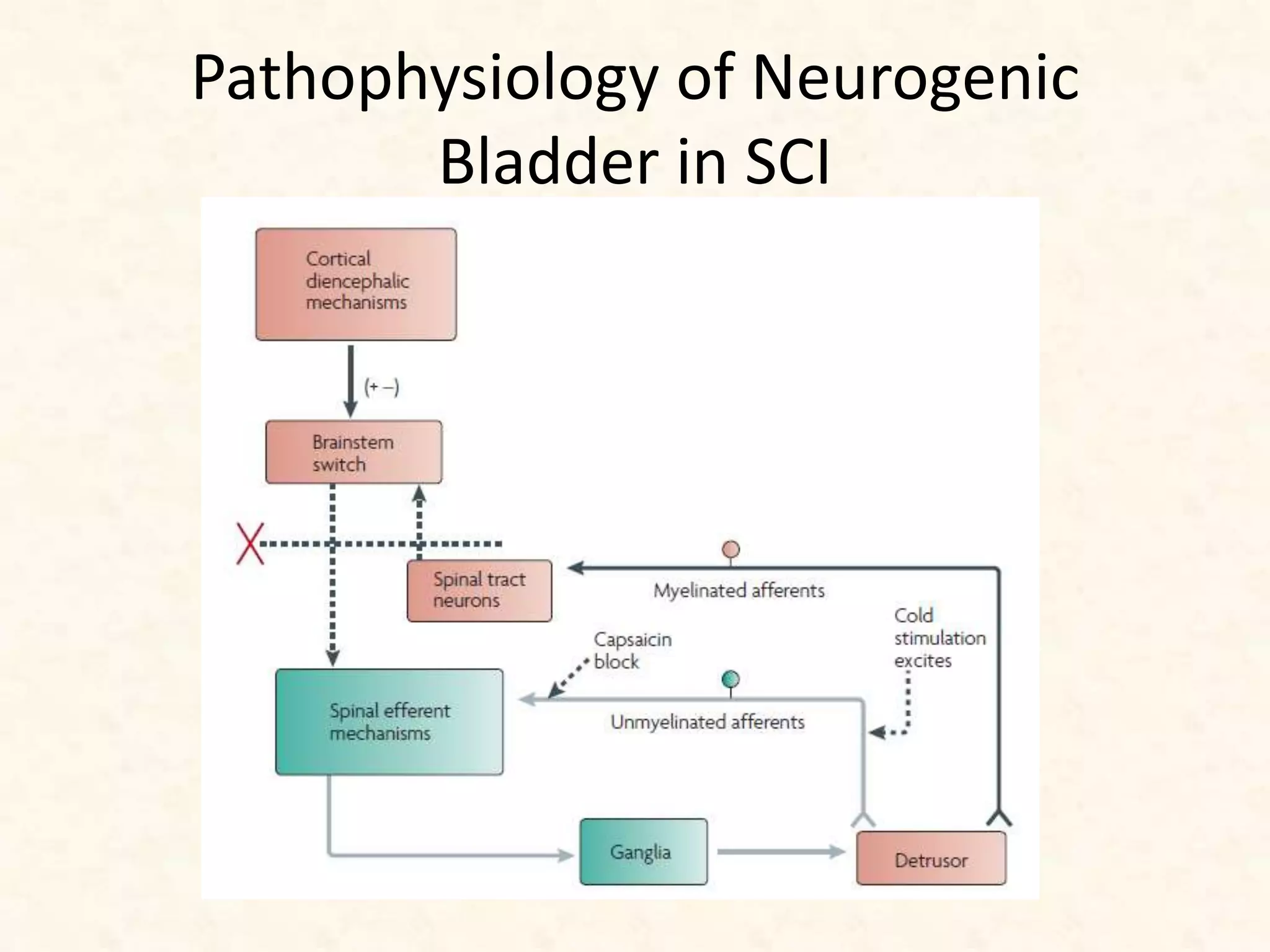
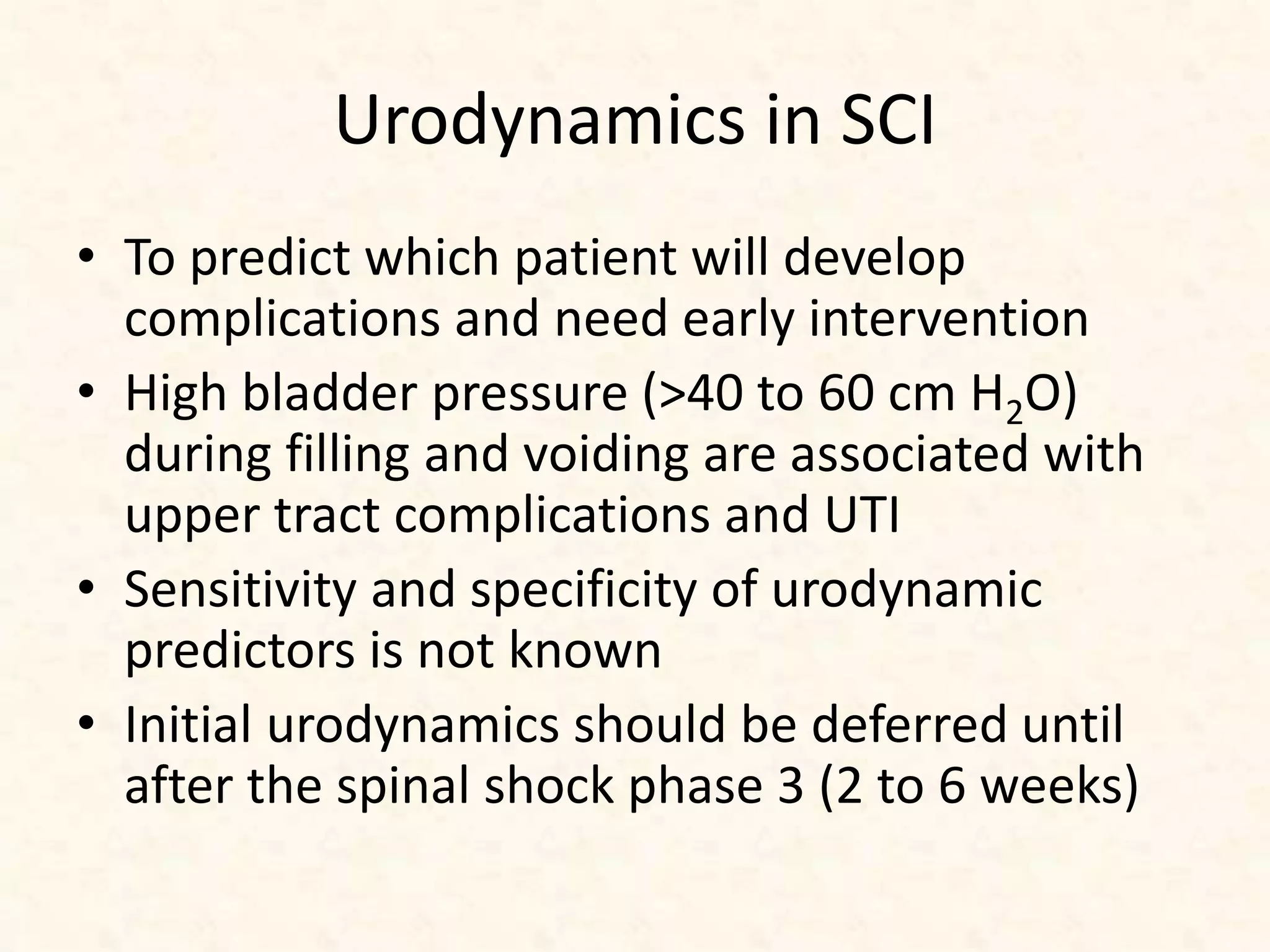
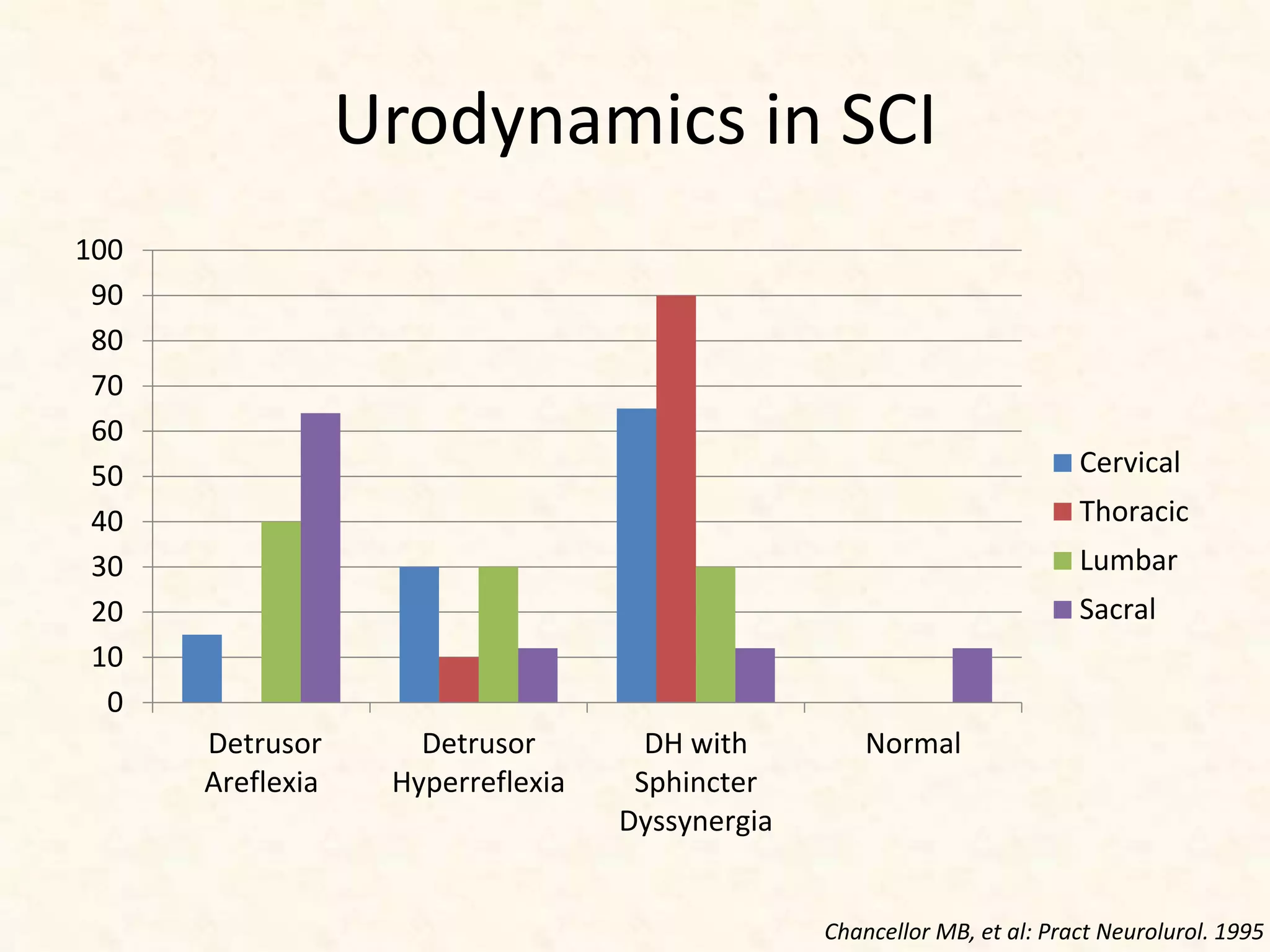
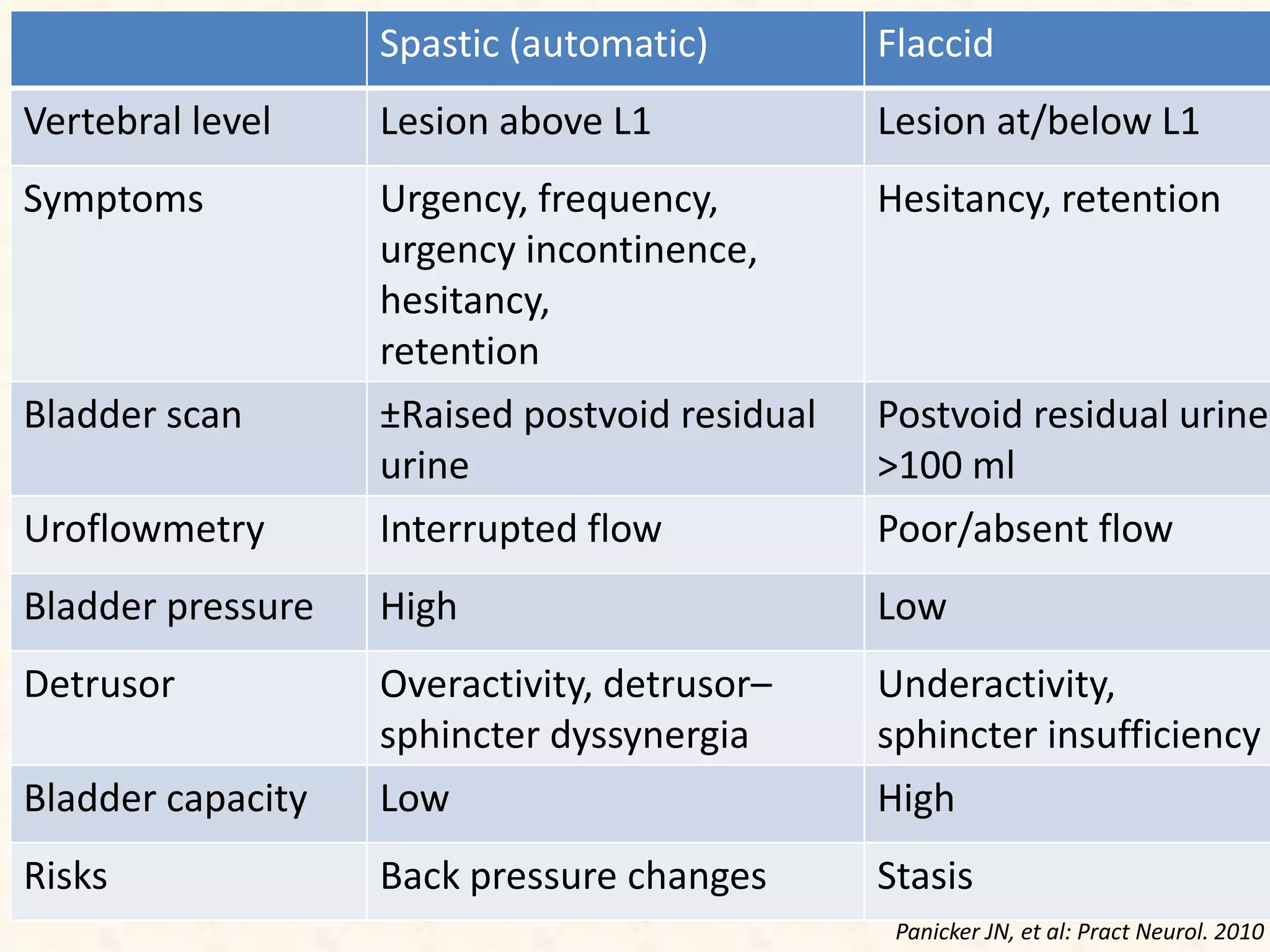
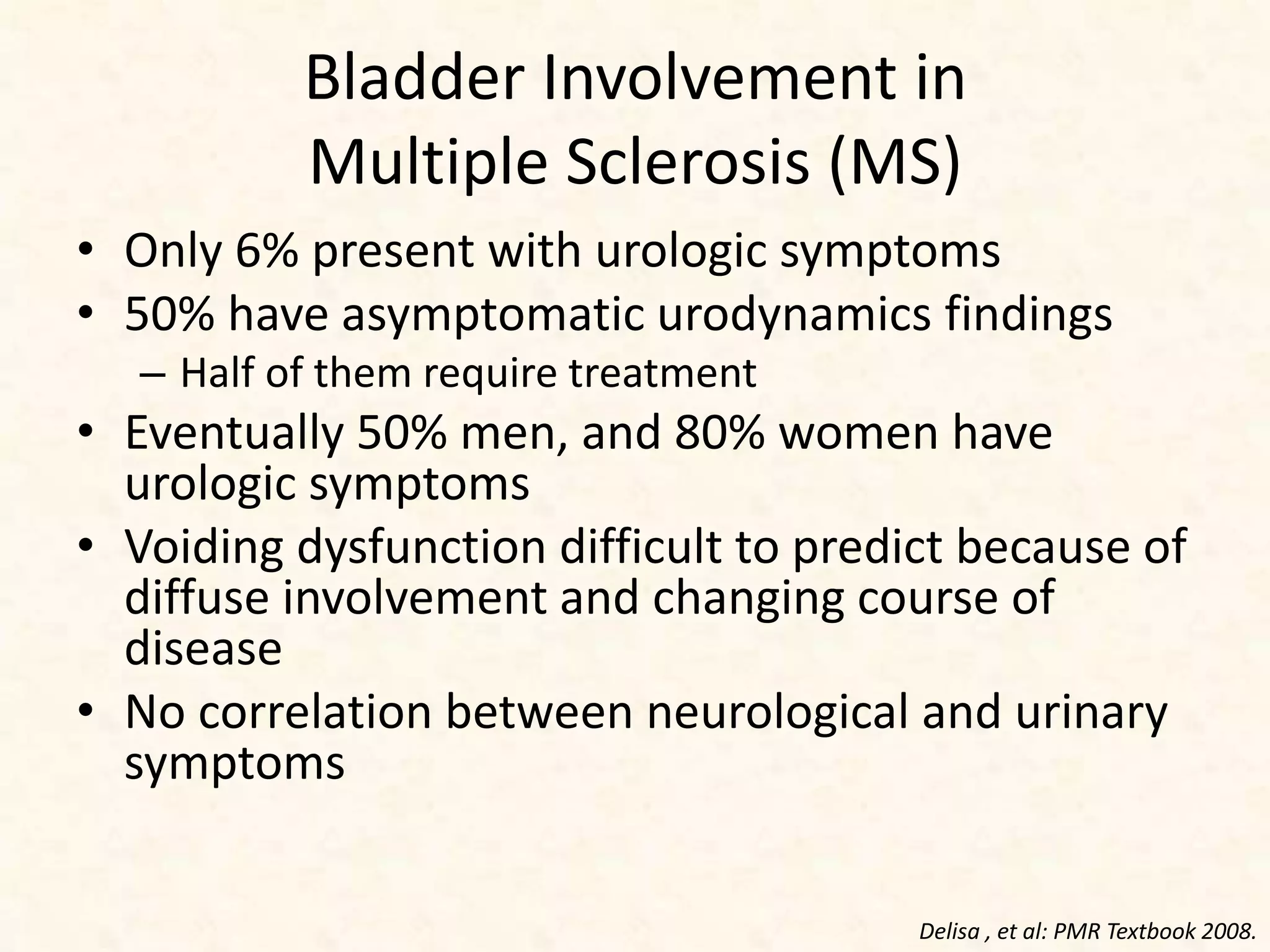
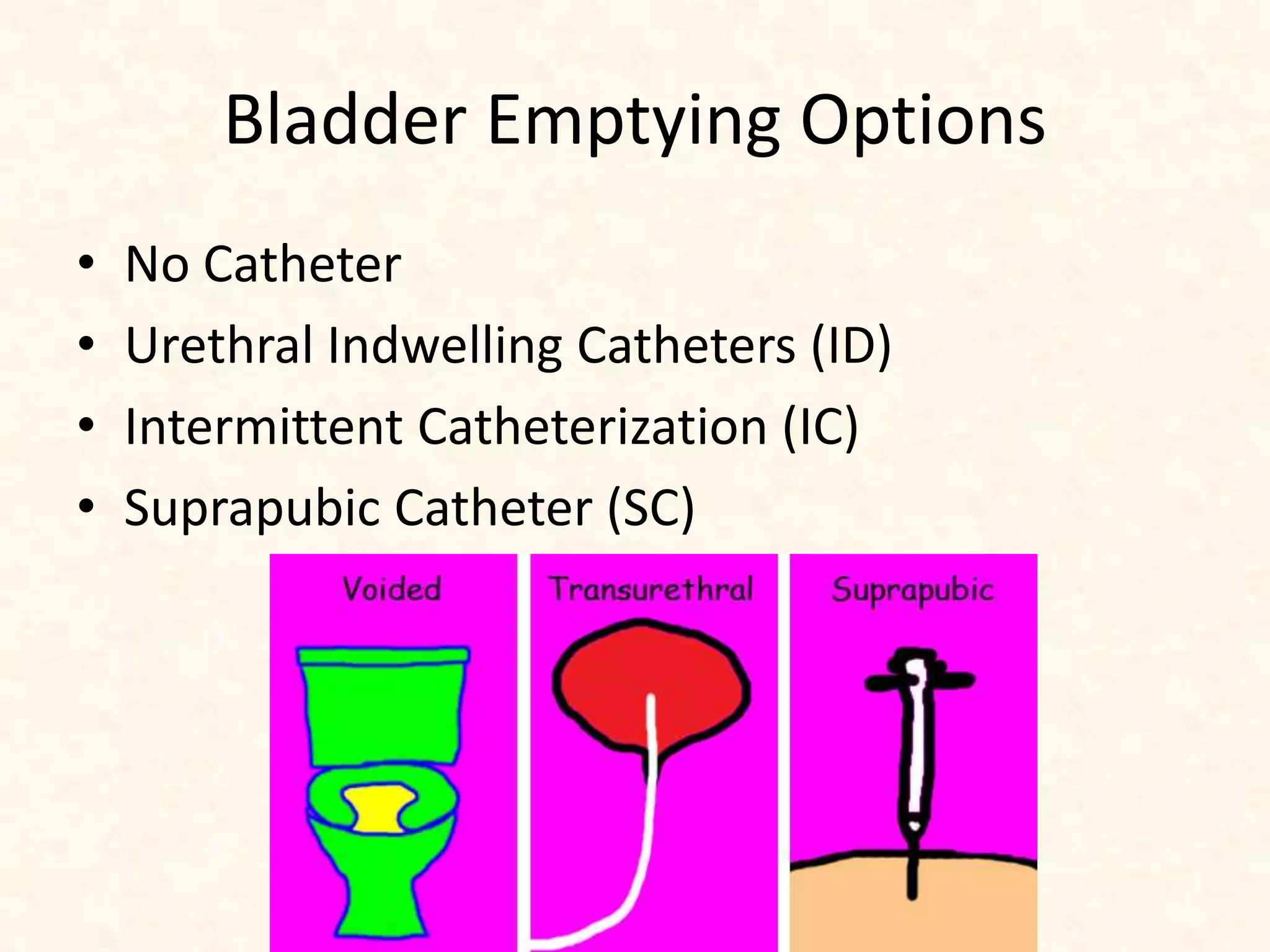
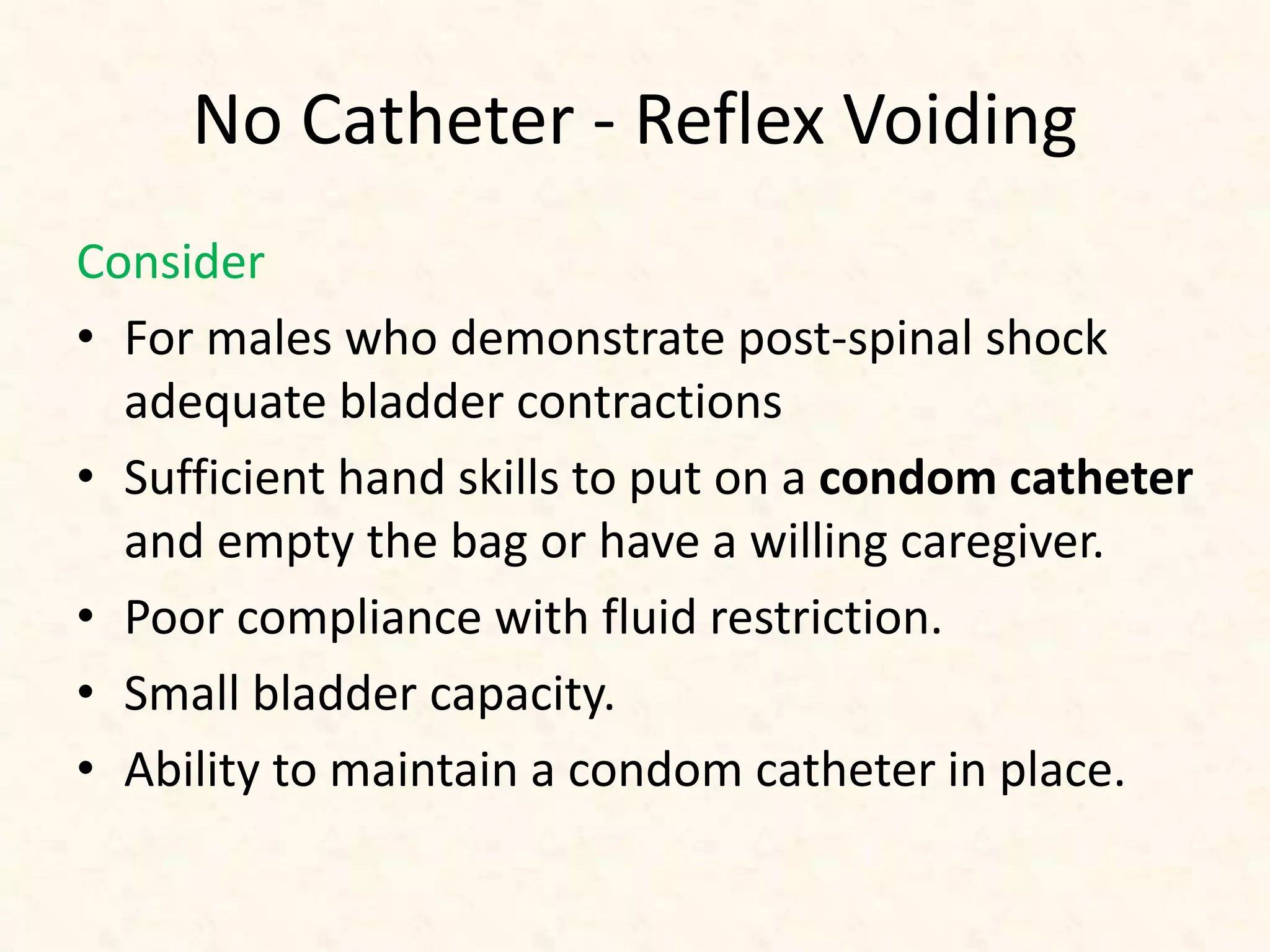
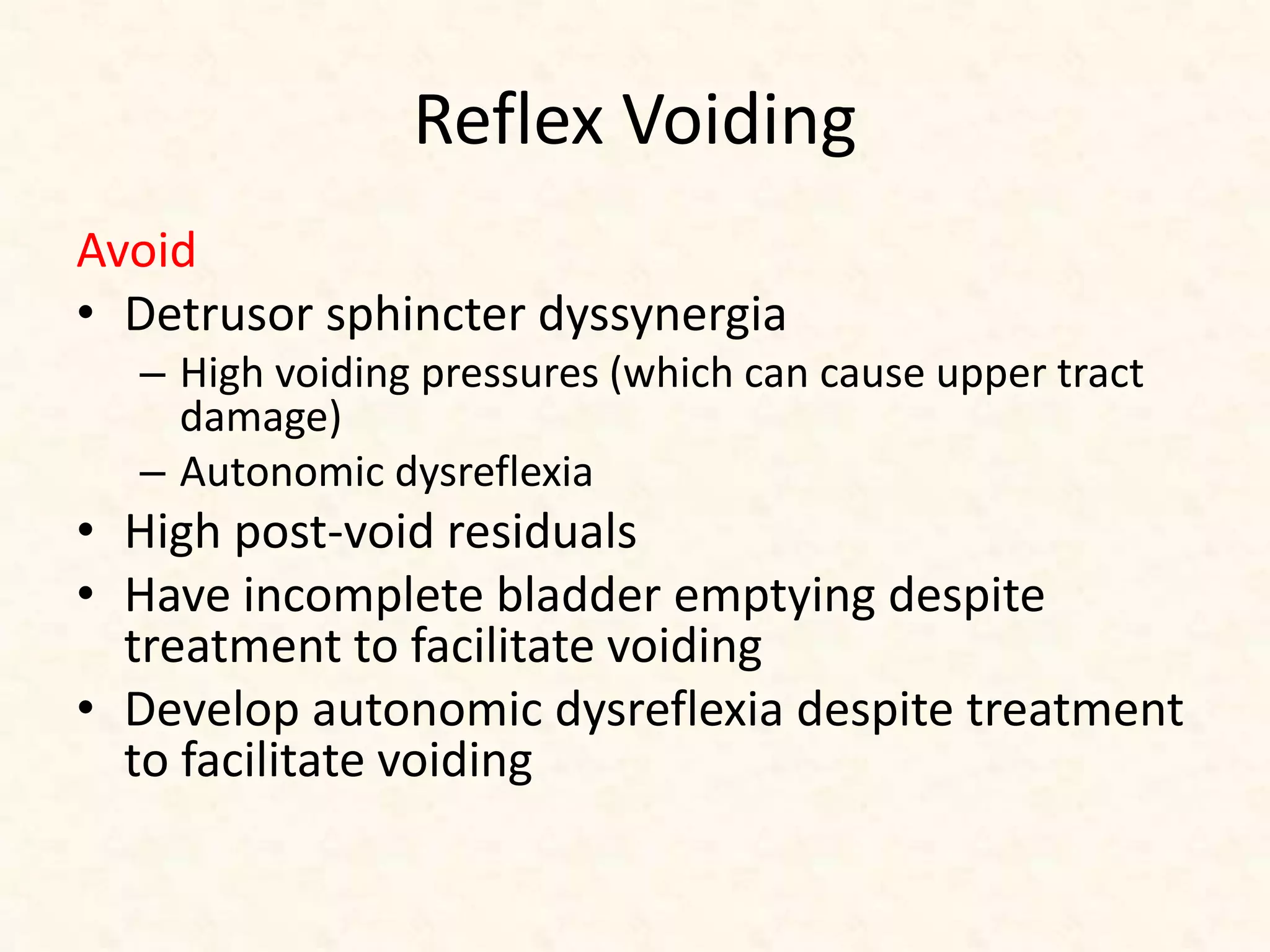
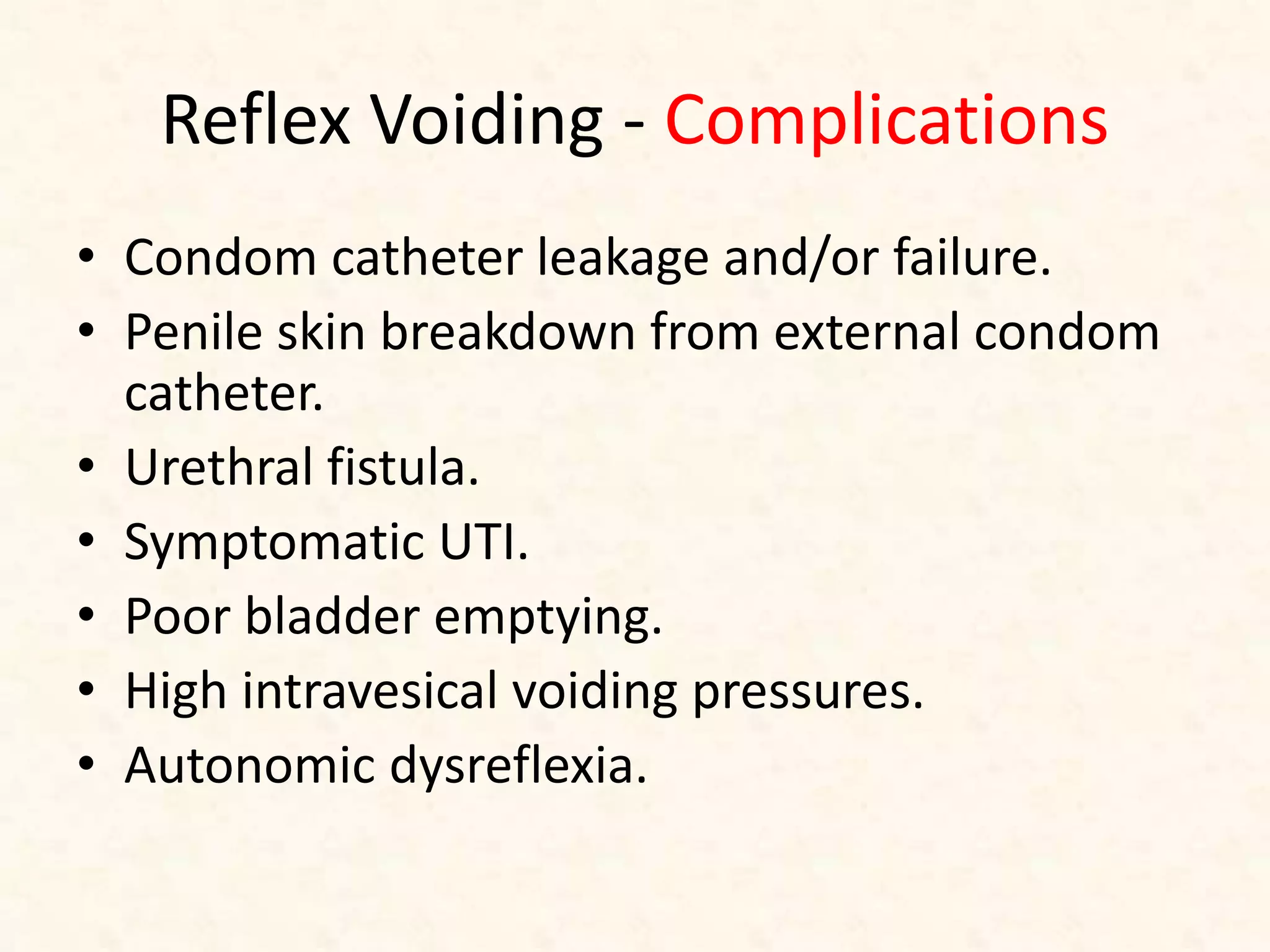
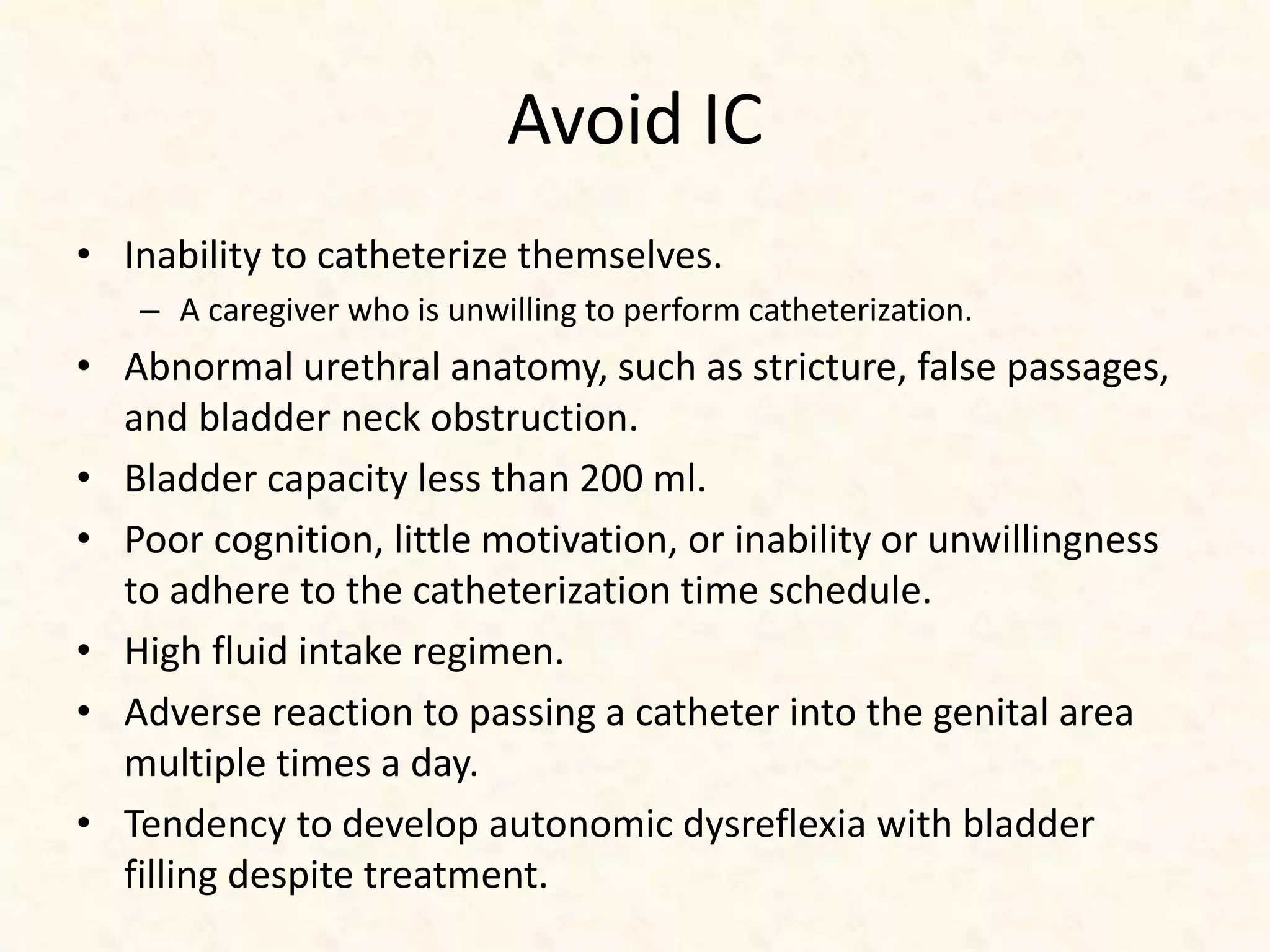
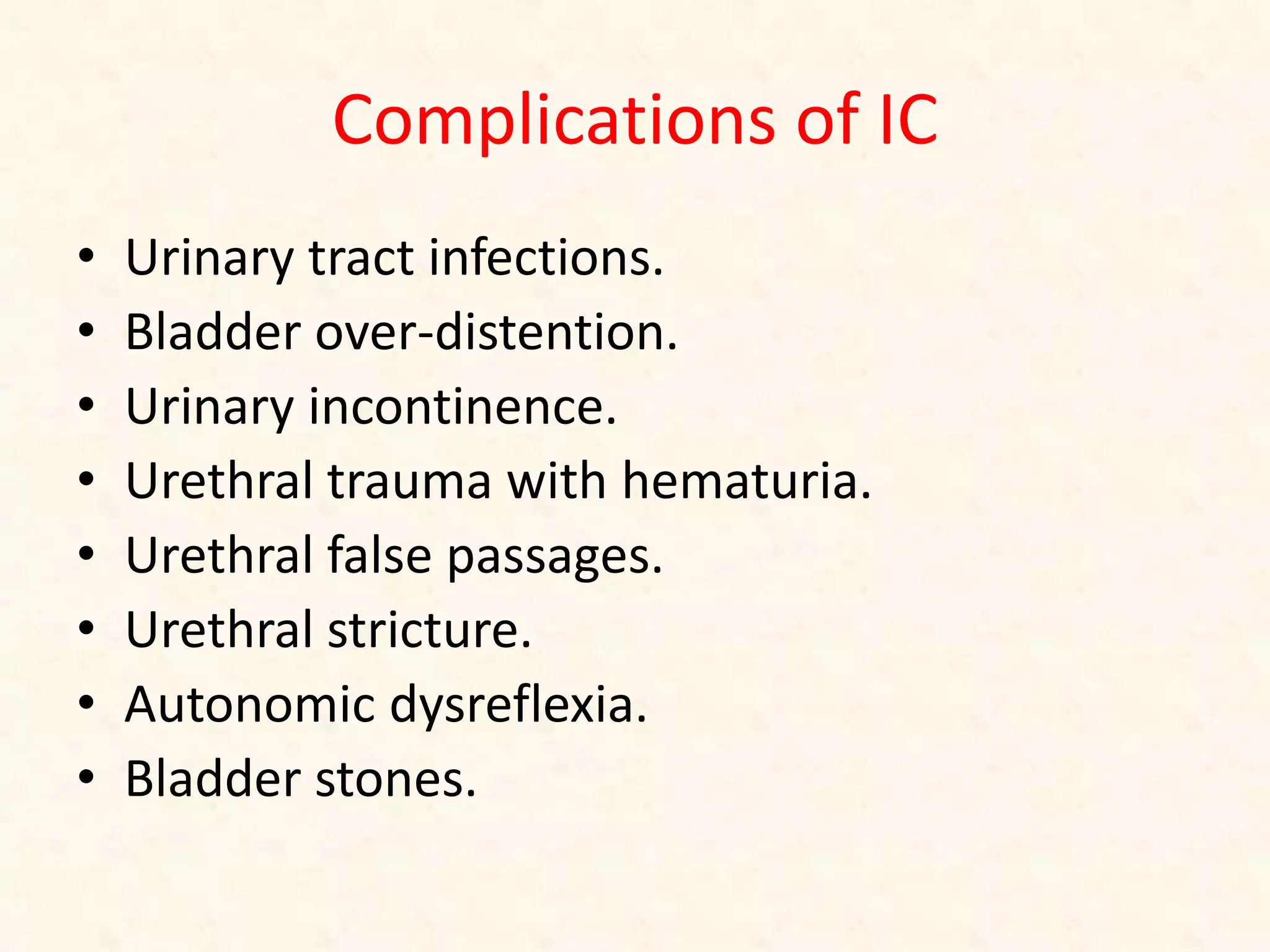
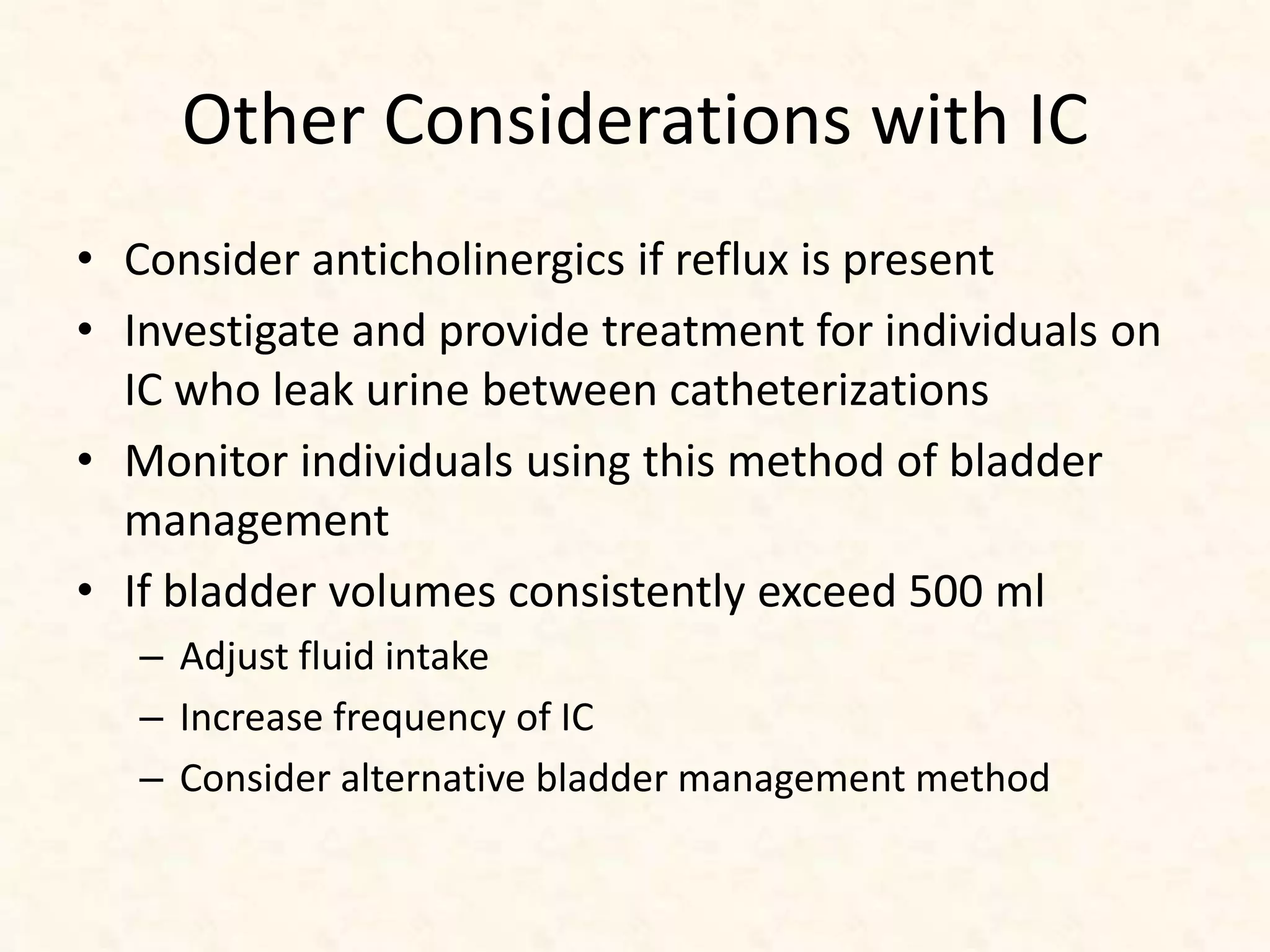
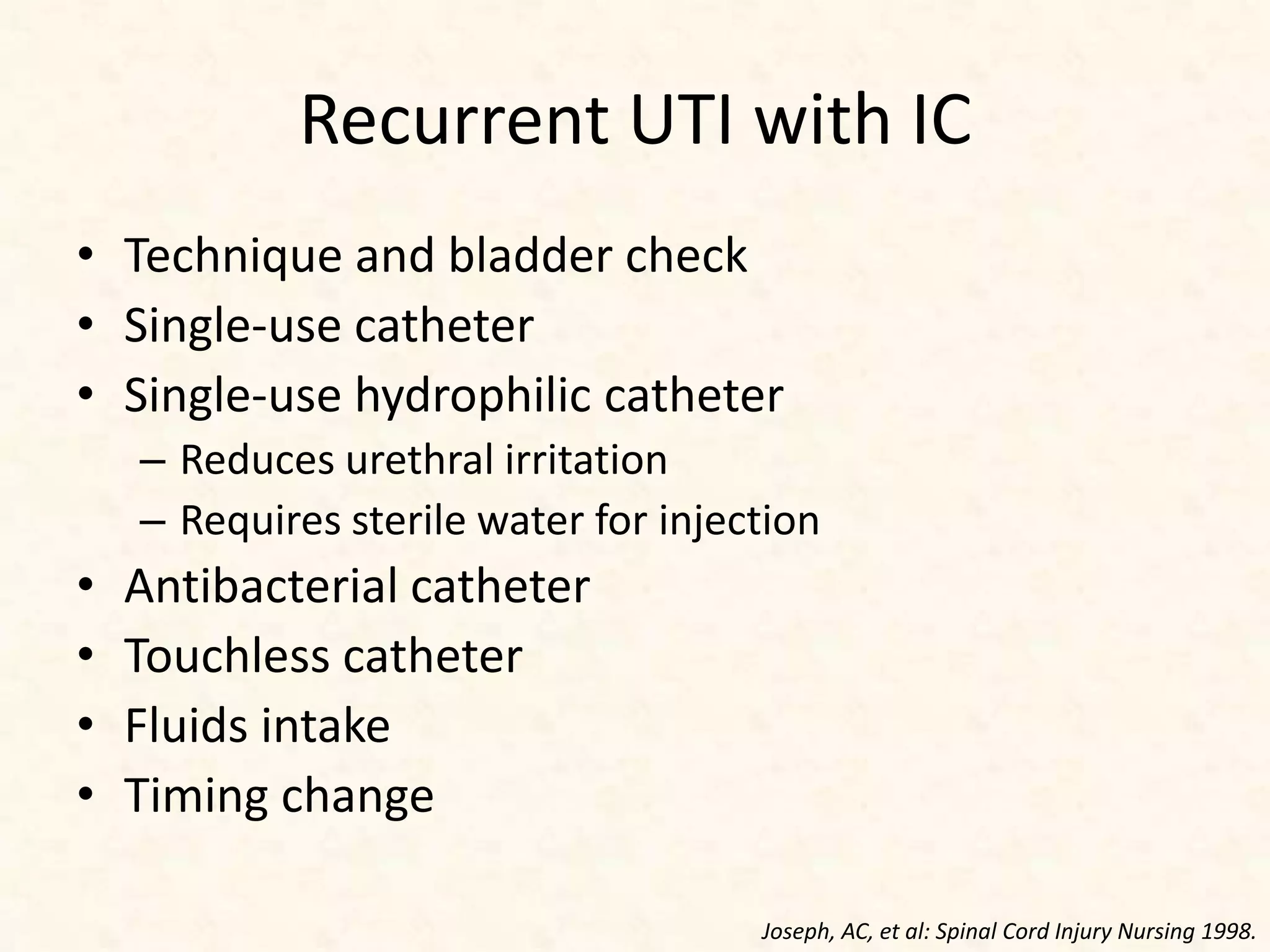
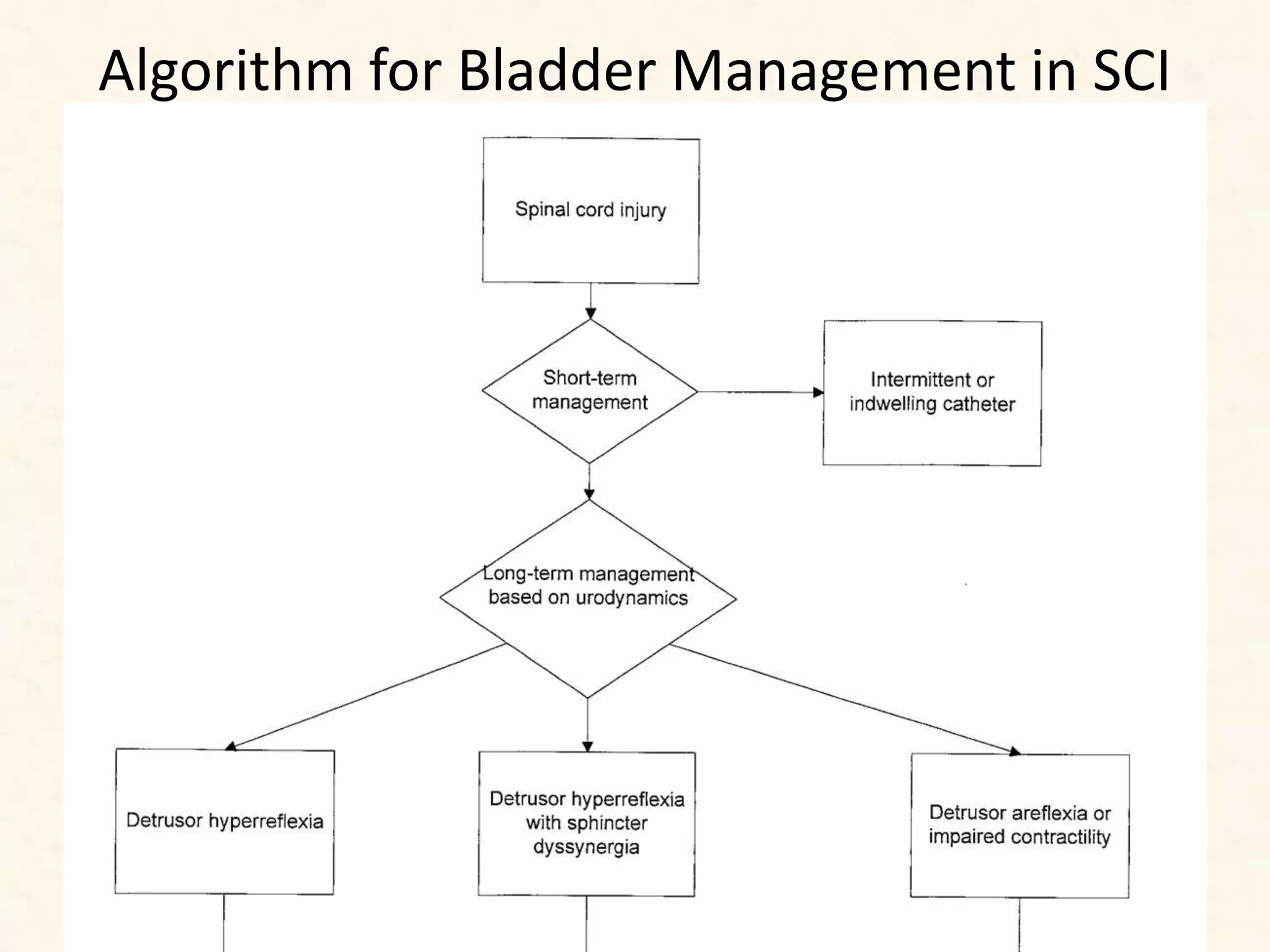
This document discusses the early management of bladder dysfunction following spinal cord injury (SCI), highlighting the significant urinary complications associated with both traumatic and non-traumatic SCI. It details the phases of bladder response post-injury, the risks of autonomic dysreflexia, and various bladder management strategies such as intermittent catheterization and suprapubic catheterization. Additionally, it emphasizes the importance of early intervention through urodynamics to predict complications and optimize treatment outcomes.