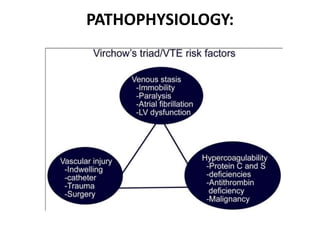
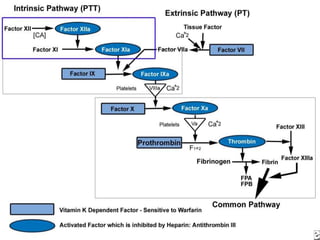
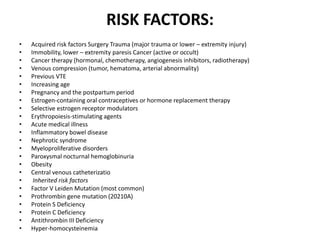
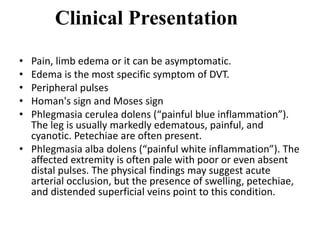
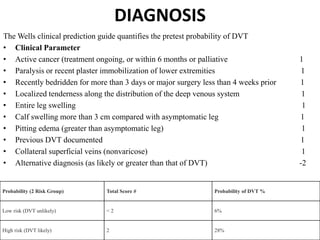
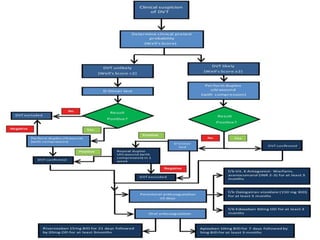
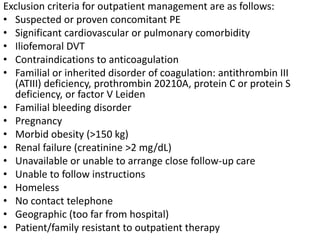
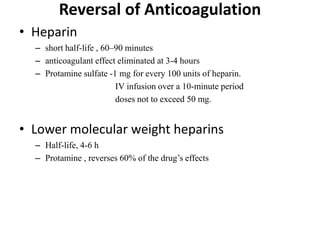
The document discusses deep venous thrombosis (DVT), detailing its epidemiology, pathophysiology, risk factors, clinical presentation, and diagnosis including the Wells clinical prediction guide. It outlines prophylaxis methods, anticoagulation therapy, complications, and treatment options such as thrombolysis and surgical interventions. Additional considerations for managing upper extremity DVT, the potential for recurrent episodes, and postthrombotic syndrome are also highlighted.
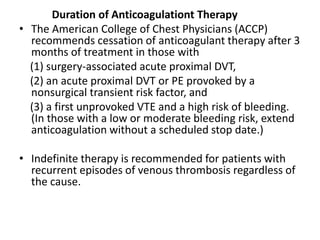
![EPIDEMIOLOGY:
• 0.75-2.69 per 1000 population
• 2-7 per 1000 in elderly
• In India, 53.6% of hospitalized patients
[surgical (61.3%), medical (44.7%)] are at-risk
for VTE, still >80% of these patients do not
receive prophylaxis.](https://image.slidesharecdn.com/deepvenousthrombosisppt-200325101826/85/Deep-venous-thrombosis-ppt-2-320.jpg)
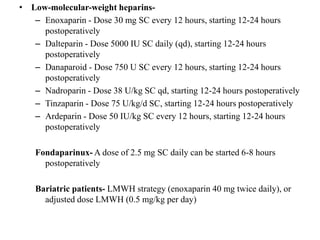
![Mechanical Methods
Passive devices- Graduated compression (elastic) stockings (GCS)
Active devices- Intermittent pneumatic compression [IPC]) devices
The use of GCS and IPC devices is recommended primarily as an adjunct to anticoagulant-based
prophylaxis in moderate to high risk patients.
Pharmacologic Methods
Aspirin- Prevent recurrent VTE in patients with an unprovoked proximal DVT following anticoagulation
cessation.
Warfarin- Started the night before surgery and continued postoperatively during the discharge period.
Heparin- Postoperative DVT prophylaxis by administering a bolus of 5000 U every 8 hours
.](https://image.slidesharecdn.com/deepvenousthrombosisppt-200325101826/85/Deep-venous-thrombosis-ppt-7-320.jpg)

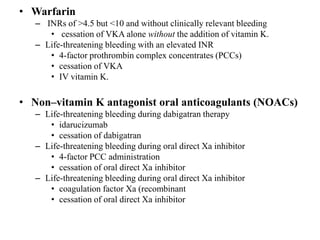
![• The guidelines on optimal management of
anticoagulation therapy for venous
thromboembolism
(released on November 7, 2018, by the American Society of
Hematology (ASH)
– For patients at low to moderate risk of recurrent VTE who
require interruption of VKA therapy for invasive procedures, the
ASH guideline panel recommends against periprocedural
bridging with LMWH or UHF in favour of interruption of VKA
alone
– For patients receiving anticoagulation therapy for VTE who
survive an episode of major bleeding, the ASH guideline panel
suggests resumption of oral anticoagulation therapy within 90
days rather than discontinuation of oral anticoagulation therapy
– For patients requiring administration of inhibitors or inducers of
P-glycoprotein (P-gp) or strong inhibitors or inducers of
cytochrome P450 (CYP) enzymes, the ASH guideline panel
suggests using an alternative anticoagulant (such as vitamin K
antagonist [VKA] or LMWH) rather than a direct oral
anticoagulant (DOAC) for the treatment of VTE](https://image.slidesharecdn.com/deepvenousthrombosisppt-200325101826/85/Deep-venous-thrombosis-ppt-19-320.jpg)