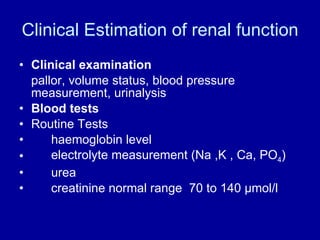
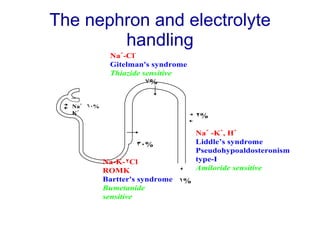
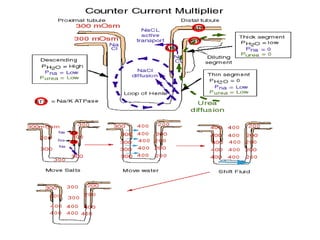
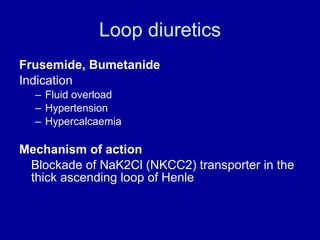
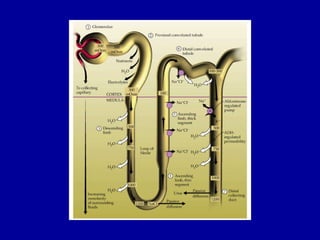
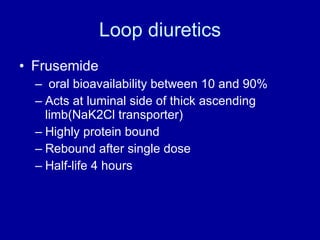
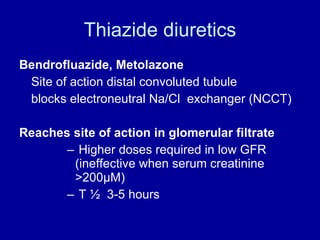
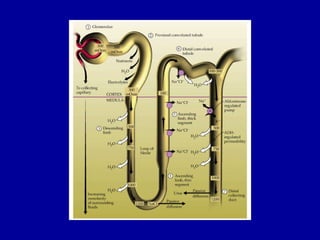
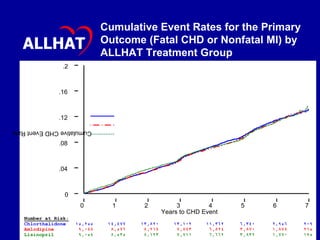
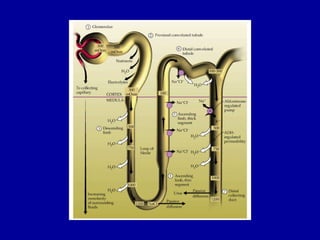
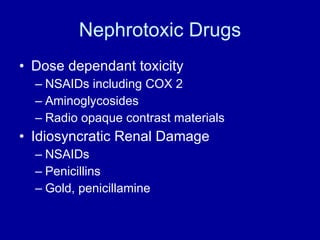
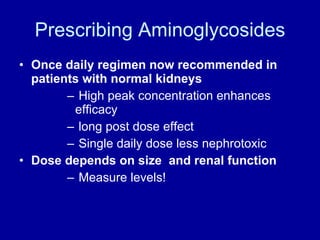
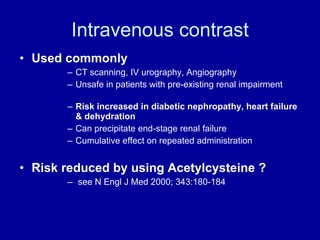
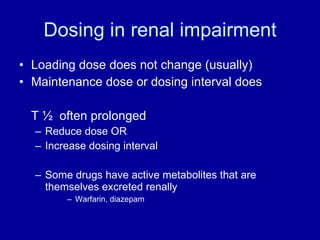
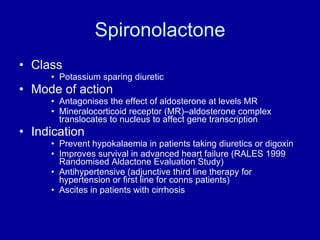
The document discusses drugs and their effects on the kidney. It covers normal kidney function, estimation of renal function, loop and thiazide diuretics, nephrotoxic drugs such as NSAIDs and aminoglycosides, and prescribing considerations in kidney disease. The ALLHAT trial found thiazide-type diuretics were superior to other antihypertensives in preventing cardiovascular disease due to their lower cost and greater efficacy.