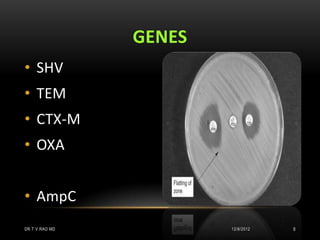
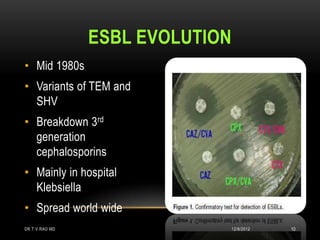
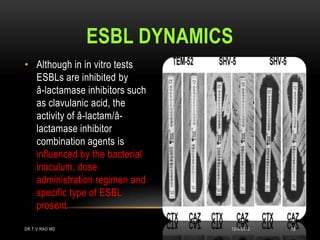
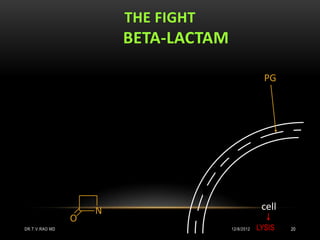
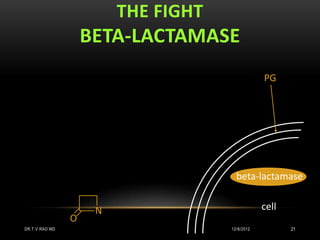
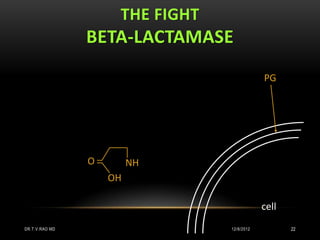
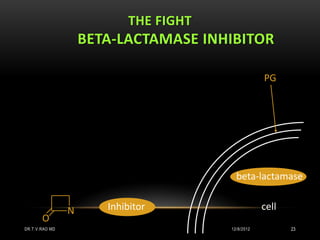
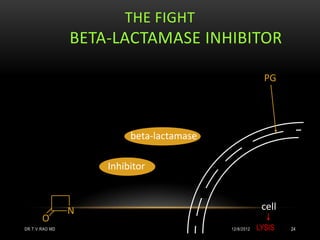
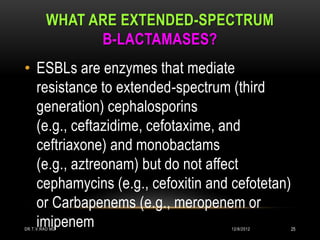
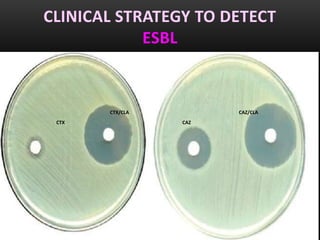
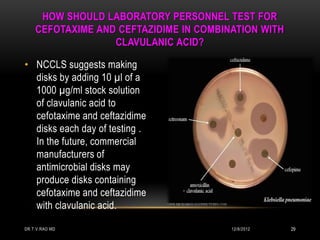
This document discusses drug resistant gram-negative bacteria. It notes that there are currently no new drugs to treat infections from multidrug-resistant gram-negative bacilli such as Acinetobacter baumannii and Pseudomonas aeruginosa. It also discusses extended-spectrum beta-lactamases (ESBLs) which are enzymes produced by bacteria that confer resistance to many beta-lactam antibiotics. The document provides information on detecting and confirming ESBL production in bacteria.