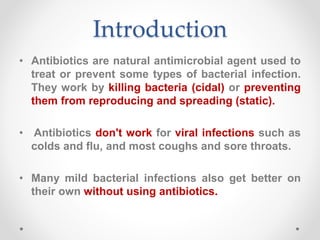
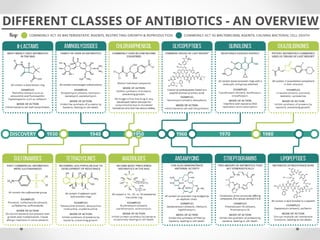
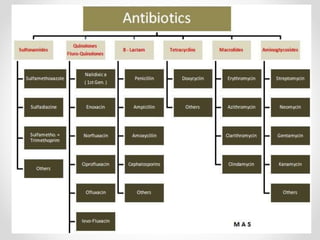
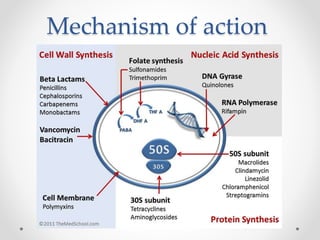
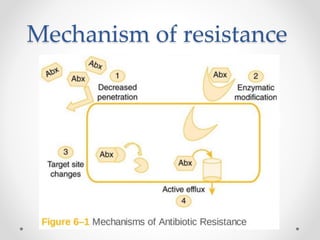
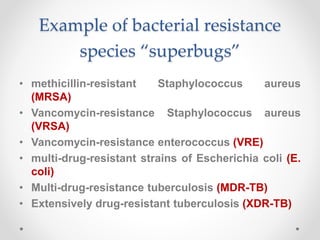
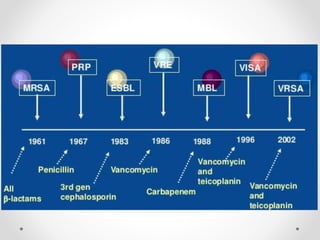
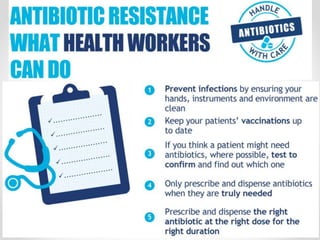
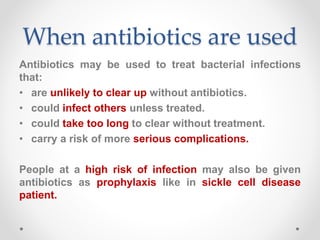
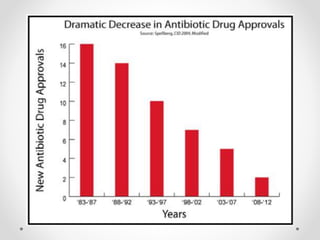
This document discusses antibiotic resistance. It begins by introducing antibiotics and their mechanisms of action in treating bacterial infections. It then defines antibiotic resistance as occurring when bacteria change in response to antibiotics, making the antibiotics ineffective. The document outlines two ways bacteria become resistant: genetic mutation or acquiring resistance from other bacteria. It provides examples of "superbugs" like MRSA, VRSA, and VRE that have developed resistance. Finally, it notes that minimizing unnecessary antibiotic use can help reduce the spread of resistance.