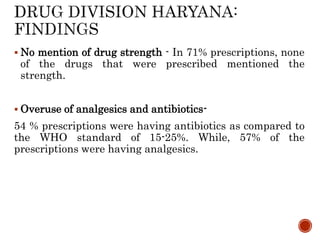
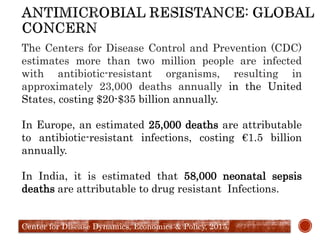
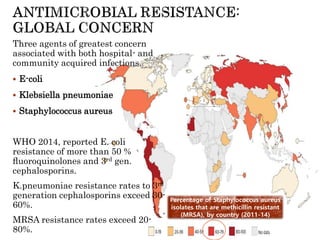
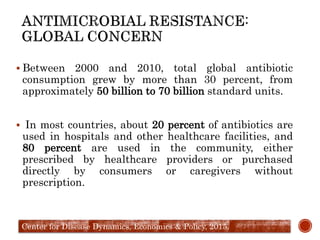
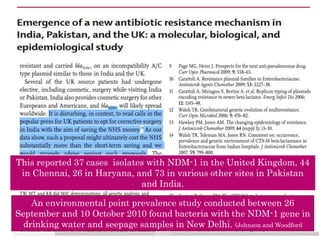
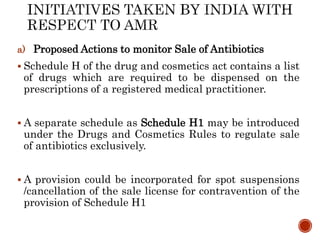
Antimicrobial resistance (AMR) poses a significant threat to public health, with microbial capabilities to resist medicine contributing to millions of infections and deaths annually worldwide. The document discusses the mechanisms and causes of AMR, highlighting concerns regarding antibiotic misuse across healthcare and agriculture, and emphasizes the urgent need for better regulations, awareness, and surveillance systems in India and globally. Initiatives like the national AMR policy and surveillance networks aim to combat this issue, but effective implementation and innovation in drug development are essential.





































![1. Identification of the pathogens / diseases of public
health importance for surveillance- Extended Spectrum-
lactamases [ESBLs] and Metallo -lactamases [MBLs], NDM-1,
MRSA & VRE
2. Creating a network of AST laboratories- In the first phase,
the following three central Govt. Hospital in Delhi will be
included for AMR surveillance.
a) Sucheta Kriplani Hospital (SKH) & Lady Hardinge Medical College
(LHMC), New Delhi
b) Dr Ram Manohar Lohia (RML) Hospital, New Delhi
c) Vardhman Mahavir Medical College (VMMC) and Safdarjung Hospital,
New Delhi](https://image.slidesharecdn.com/antimicrobialresistancenew-161218032557/85/Antimicrobial-resistance-new-50-320.jpg)