This document discusses the doctor-patient relationship and communication. It covers:
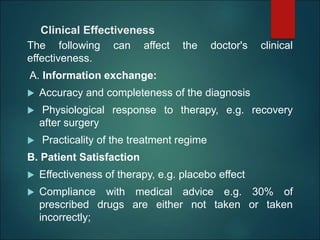
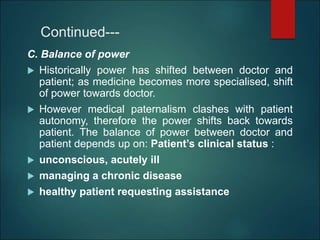
1) The core of medicine is the doctor-patient relationship, with patients expecting both a good relationship and cure. The relationship itself can be part of the therapeutic process.
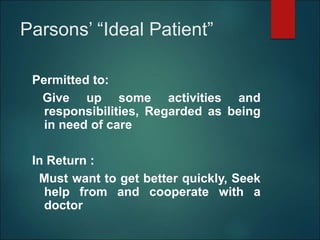
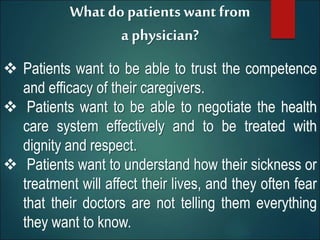
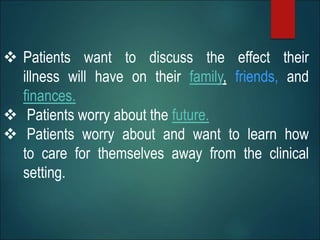
2) Patients want to trust their doctor's competence, navigate the healthcare system effectively, be treated with dignity and respect, understand how illness/treatment affects their lives, discuss impacts on family/finances, and learn self-care.
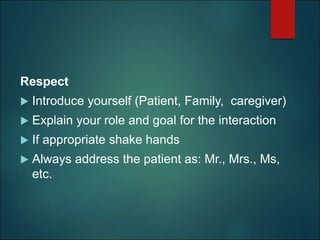
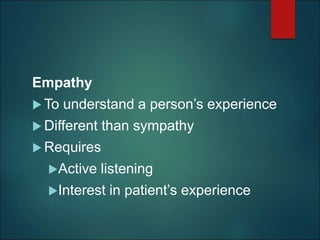
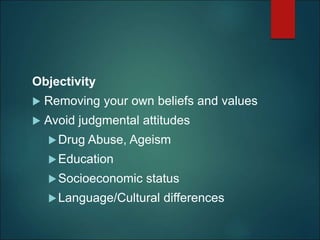
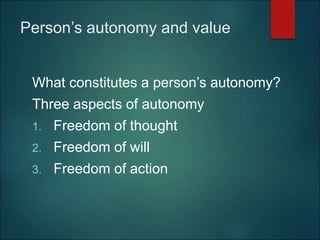
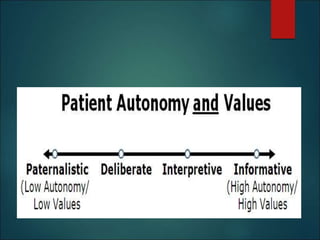
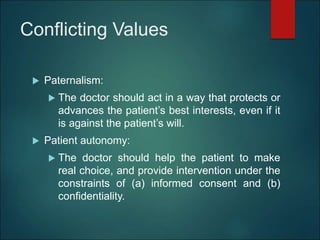
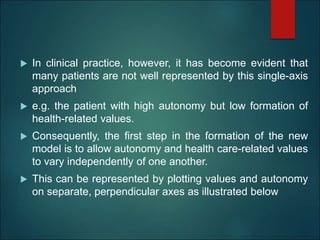
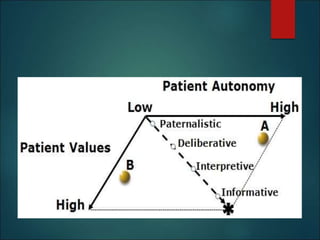
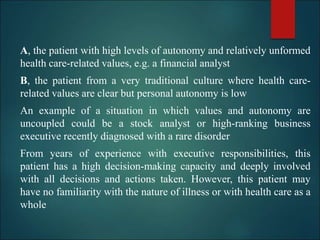
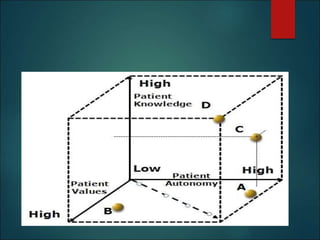
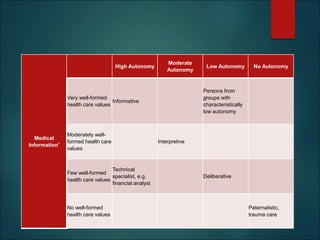
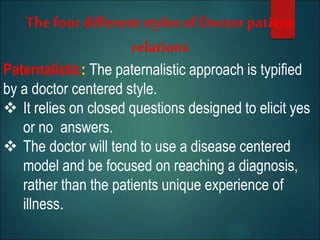
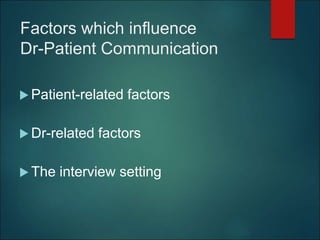
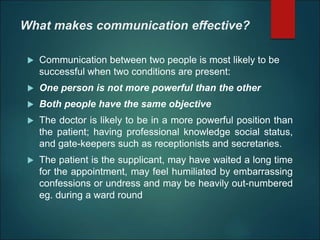
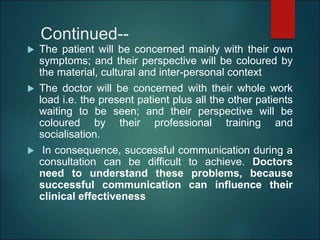
3) Effective communication is unique due to the immediate trust and vulnerability patients have with doctors during examinations. Respect, empathy, objectivity, and understanding patient autonomy and values are important.