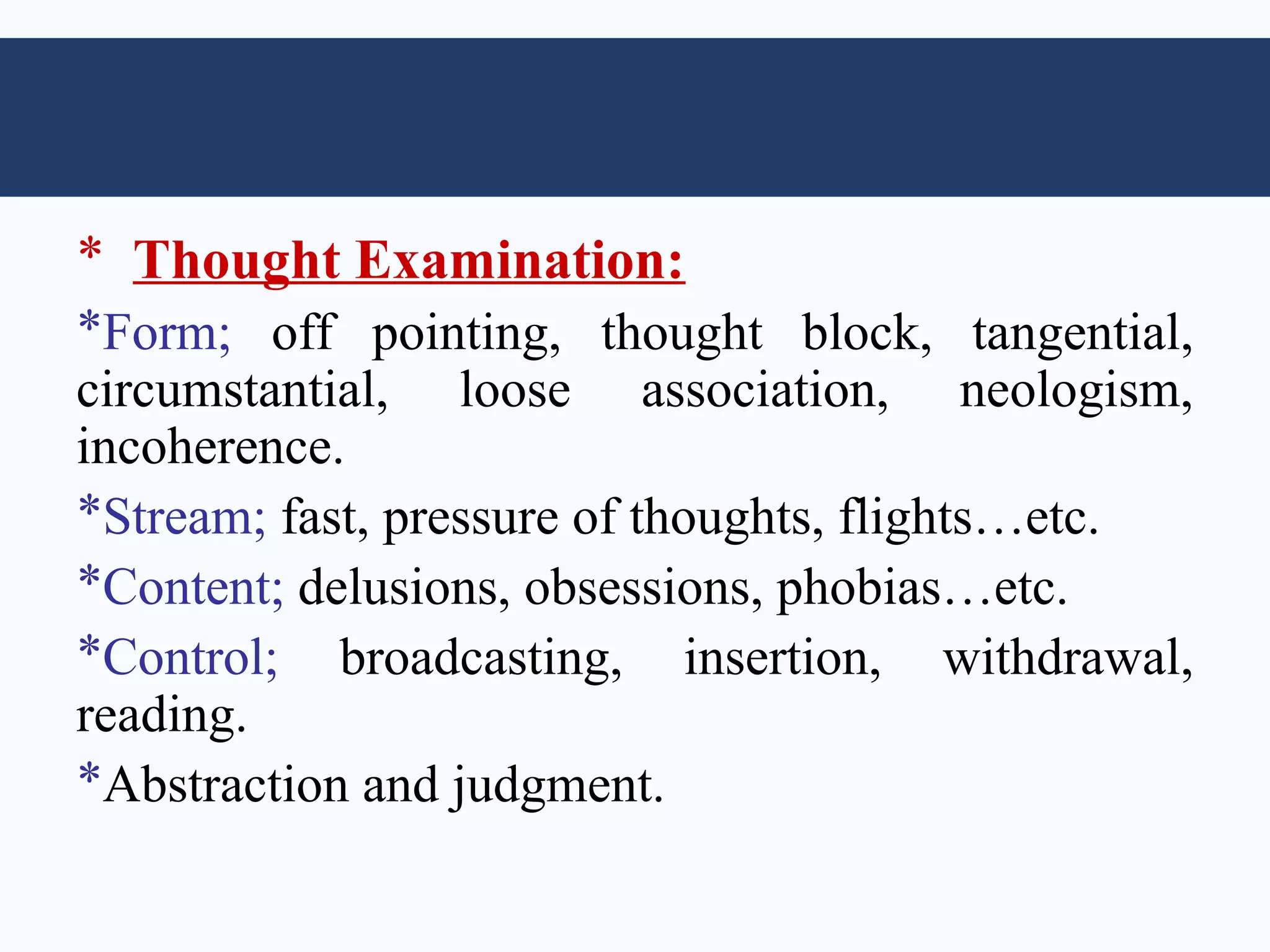
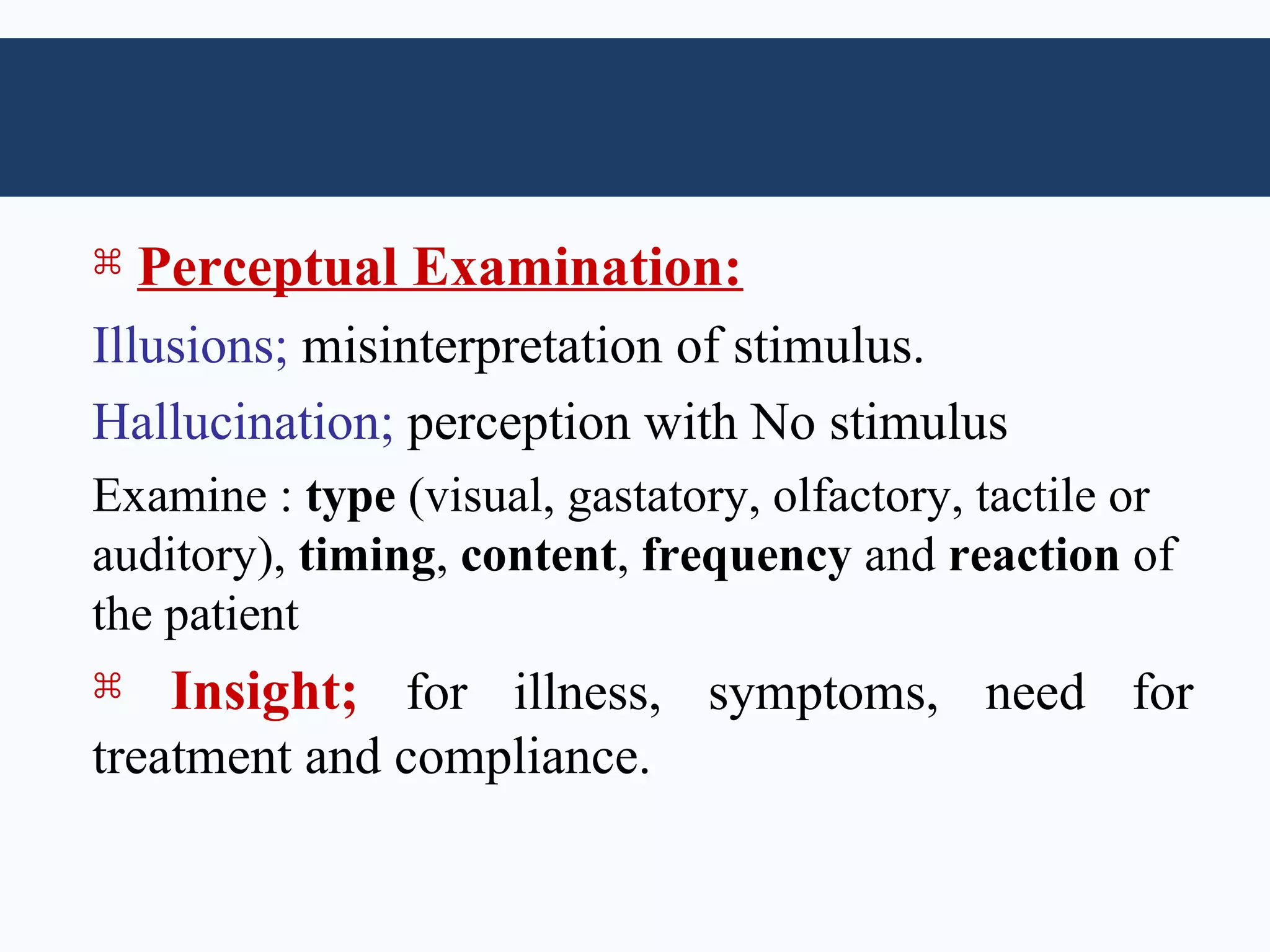
This document provides an overview of the components of a psychiatric history taking and examination. It describes collecting personal data, the patient's complaint, history of present illness, past medical and psychiatric history, personal history including development, relationships, and sexual history. It also includes obtaining a family psychiatric and medical history. The examination involves a mental status exam assessing appearance, behavior, mood, affect, speech, thought content and process, perception, and insight. The goal is to chronologically understand the patient's life and current symptoms from their perspective and an informant to make an accurate diagnosis.