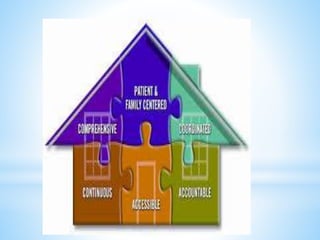
1) Patient-centered care is a philosophy that encourages shared control of medical decisions between the patient and doctor and focuses on treating the whole patient, not just their disease.
2) The concept developed in the 1950s and key components include understanding the patient's experience of illness and social context, finding common ground on treatment goals, and enhancing the patient-doctor relationship.
3) Benefits of patient-centered care include improved patient satisfaction and adherence, better health outcomes, and decreased medical litigation. While it may take more time initially, average visit lengths are not significantly different than conventional care.