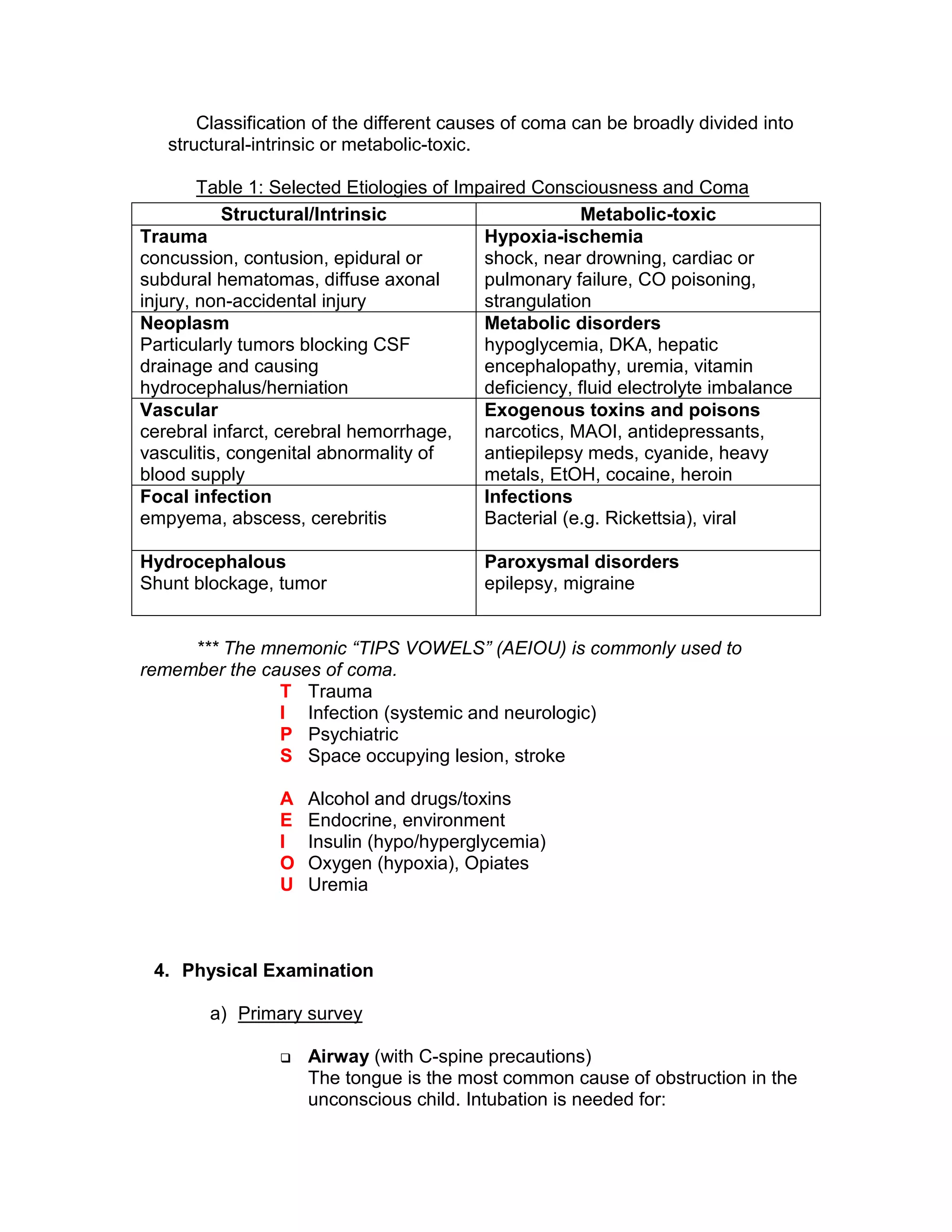
This document provides an approach to evaluating and diagnosing a comatose child. It begins with definitions of key terms like consciousness and coma. It then discusses important questions to ask about timing and associated symptoms. A differential diagnosis classification divides potential causes into structural/intrinsic and metabolic/toxic categories. The physical exam involves a primary survey of airway, breathing, circulation and disability followed by a secondary survey examining various body systems. Key investigations include laboratory tests, imaging studies like CT/MRI, lumbar puncture and EEG. The goal is to identify structural lesions, infections, toxic/metabolic derangements or other conditions causing an altered level of consciousness.