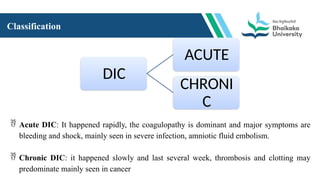
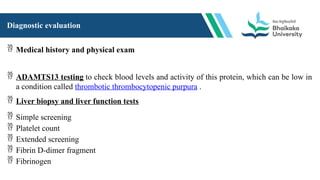
This file includes Introduction of the topic that what DIC is. it also contains definition of DIC. what are the Causes and Risk factors for this particular disease condition and how to understand the progression of DIC into the body by explanation of Pathophysiology of DIC. what kind of clinical manifestation patient may feel, which are the diagnostic evaluation and test is necessary to handle any patient having DIC. this file also having content regarding how to manage the patient including medical management, surgical management, specifically the nursing management and nutritional management.