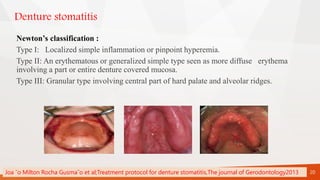
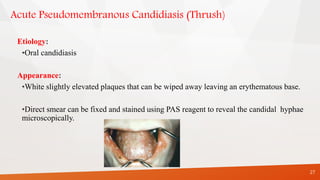
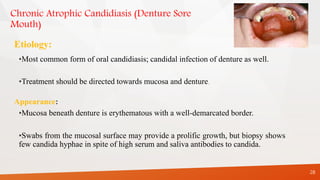
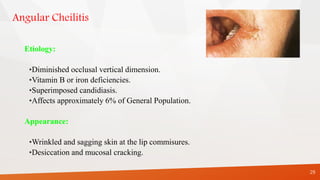
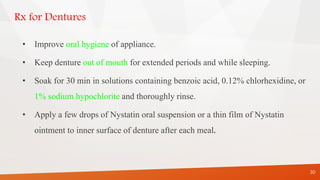
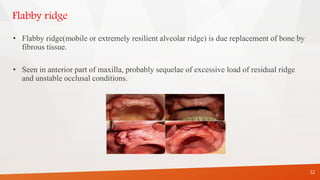
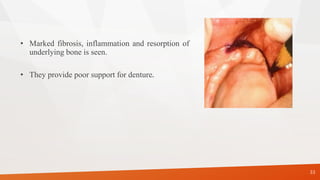
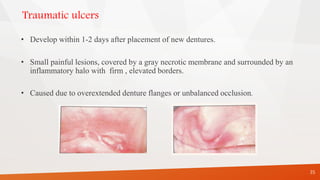
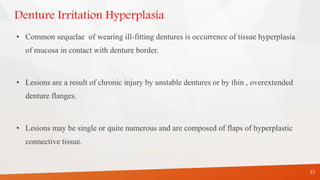
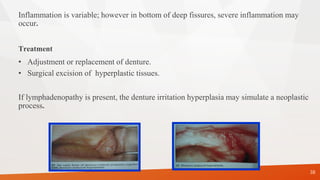
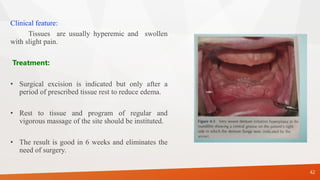
The document discusses the sequelae of wearing complete dentures. It can cause both direct and indirect effects on oral tissues. Direct sequelae include denture stomatitis, traumatic ulcers, denture irritation hyperplasia, and clicking sounds. Indirect sequelae are the atrophy of muscles and nutritional deficiencies. The document provides details on the etiology, clinical features, and management of various conditions associated with complete denture wearing. It emphasizes the importance of denture fit, oral hygiene, and follow-up care in preventing sequelae.