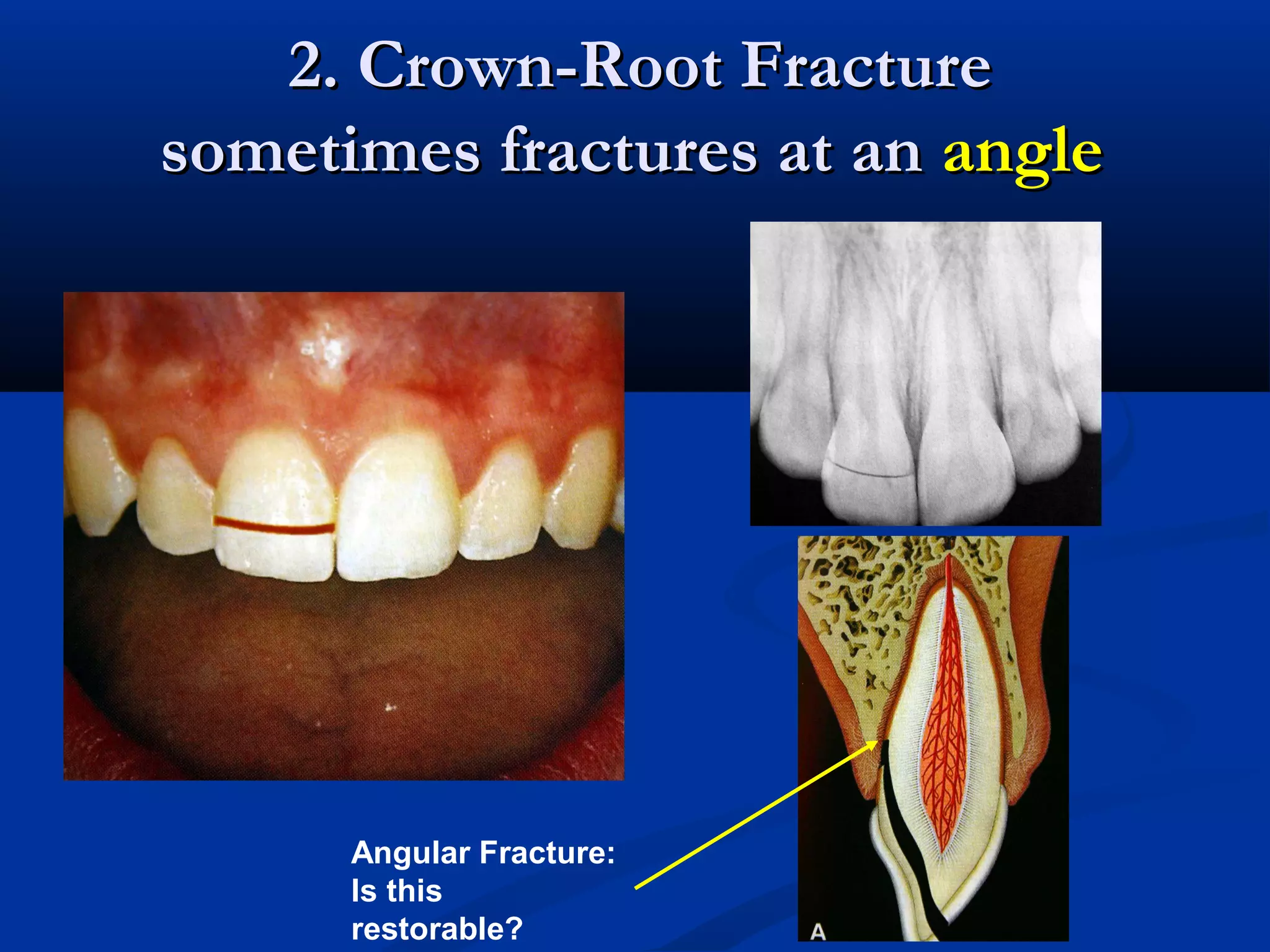
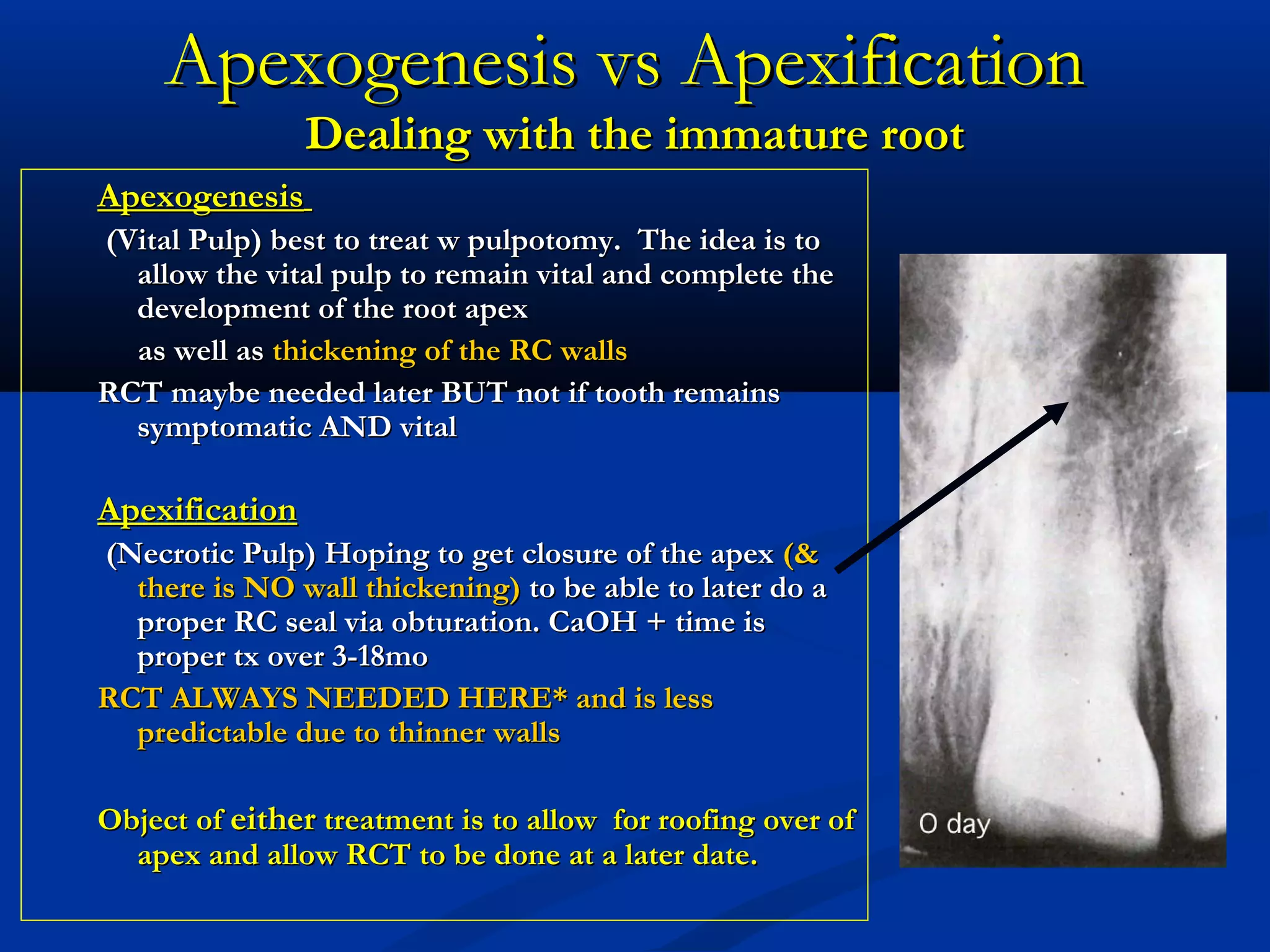
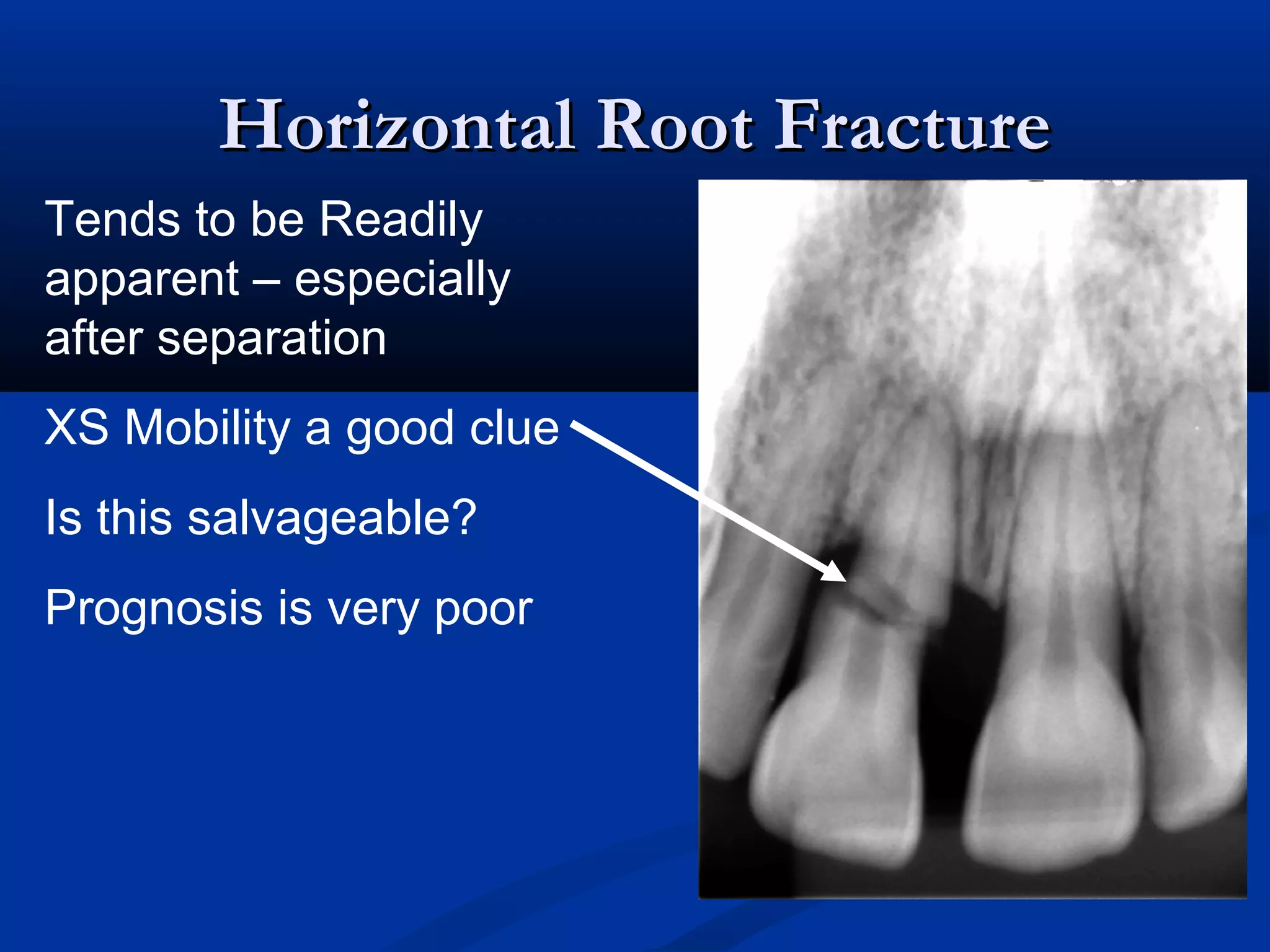
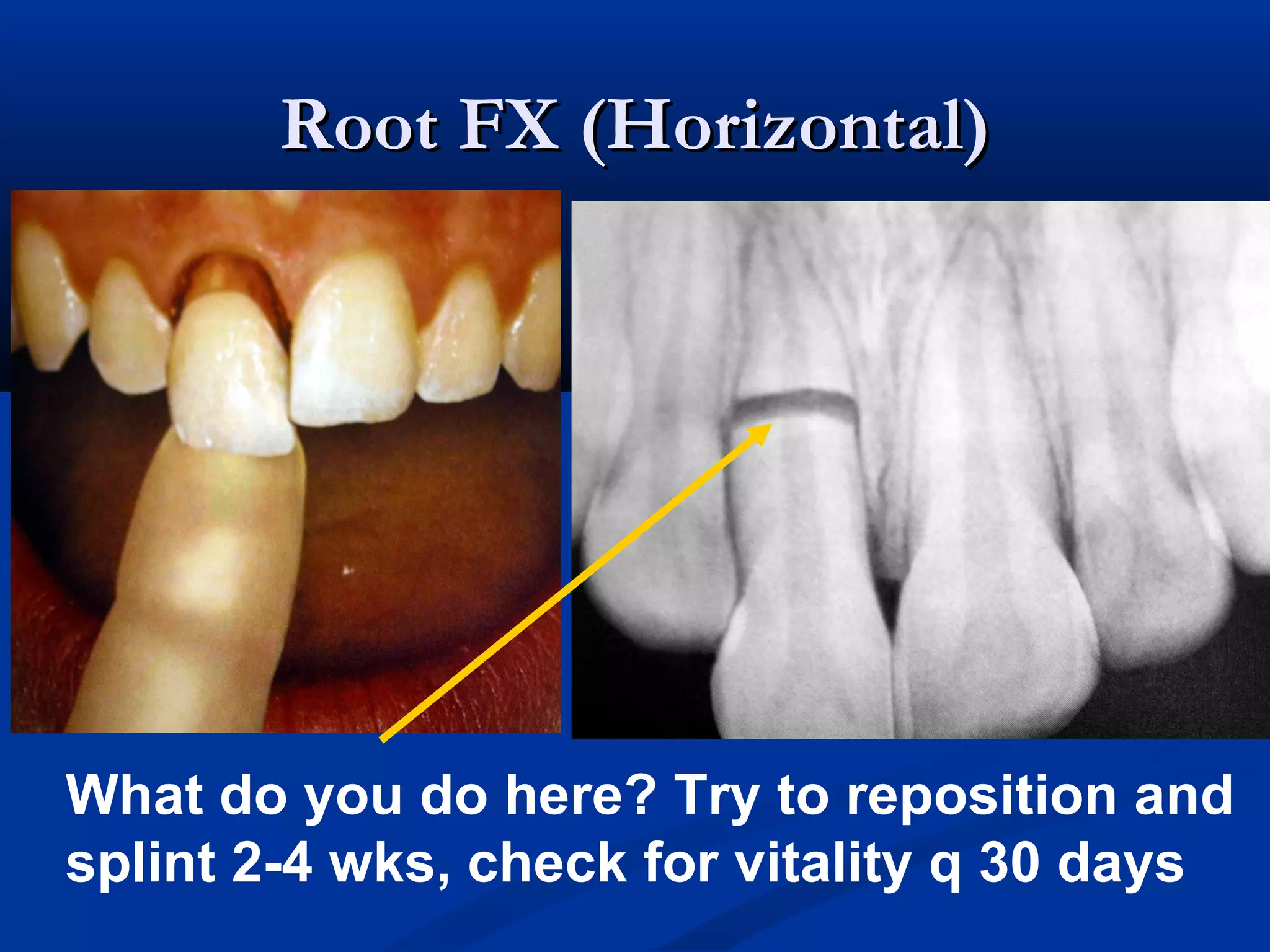
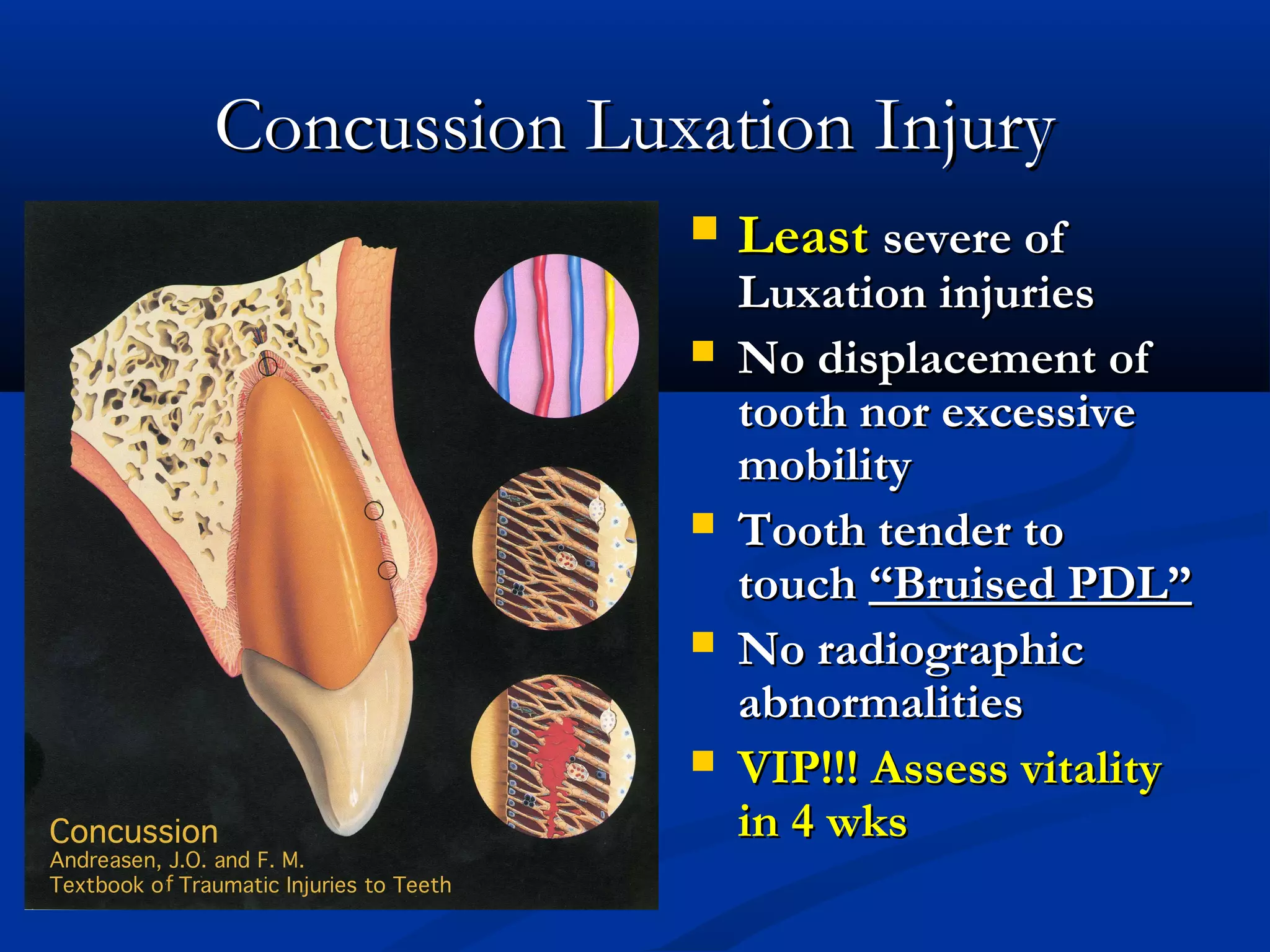
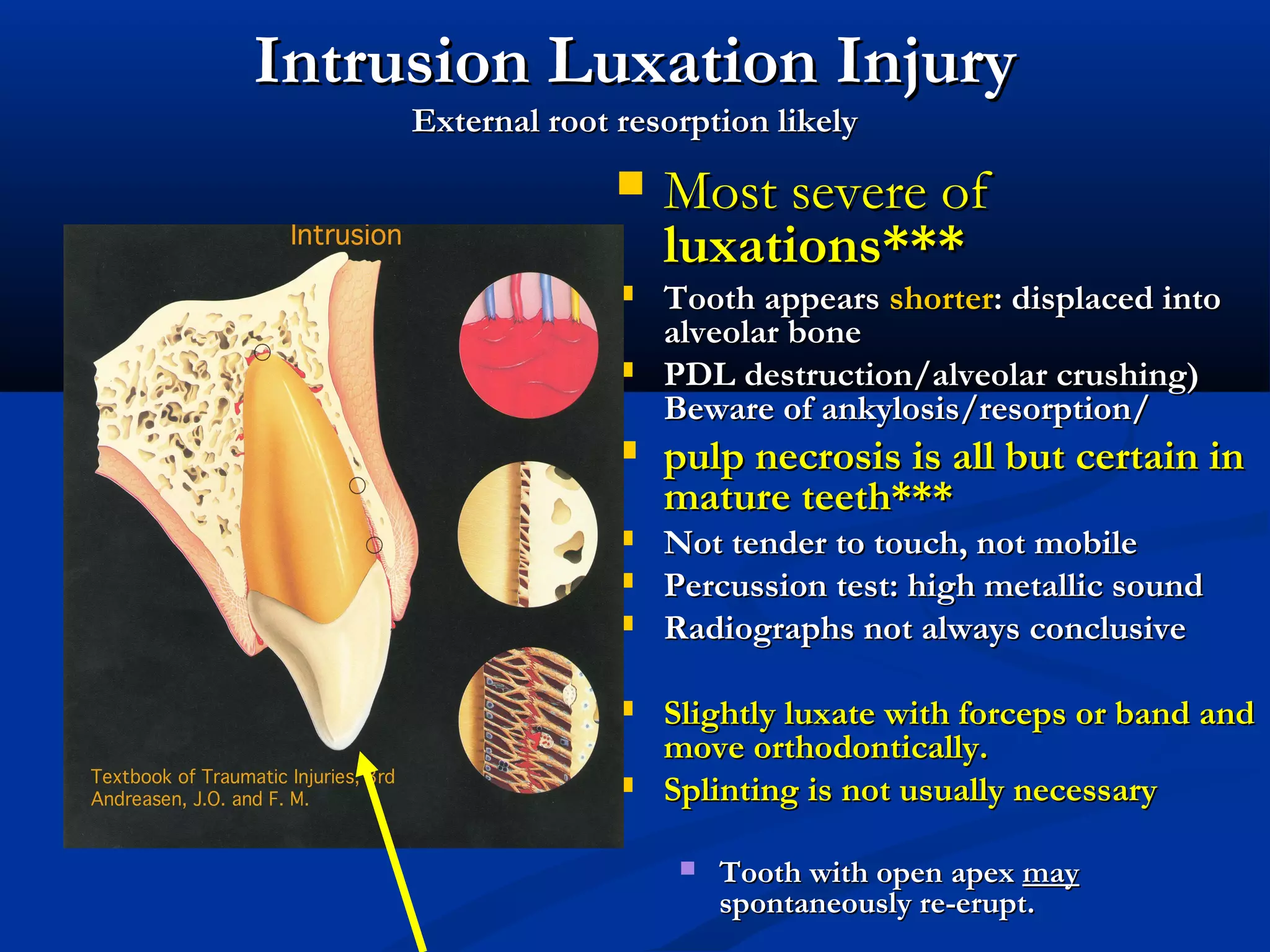
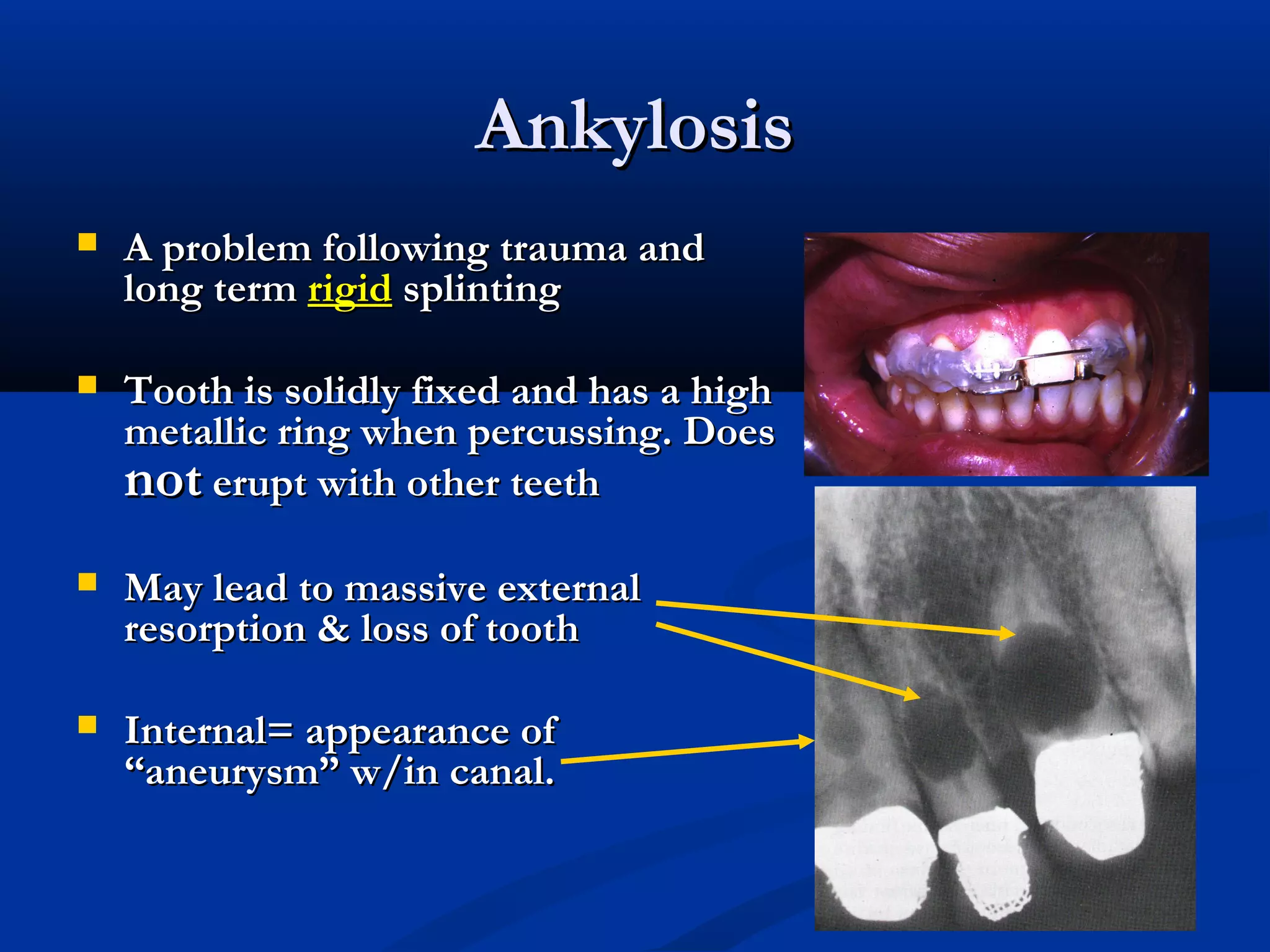
The document discusses various types of traumatic dental injuries including crown fractures, root fractures, luxation injuries, and avulsion. It provides details on diagnosing each type of injury and outlines treatment approaches. For many injury types, the goal is to maintain pulp vitality through treatments like pulpotomy or replantation after avulsion. Complications can include pulp necrosis, resorption, and ankylosis from long-term splinting. The document emphasizes the importance of rapid treatment and splinting to optimize outcomes and prevent tooth loss from traumatic injuries.