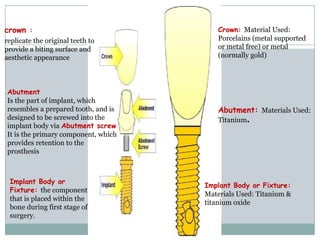
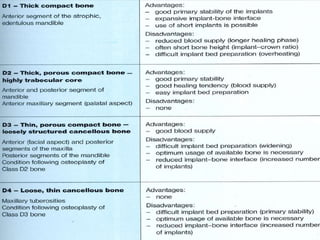
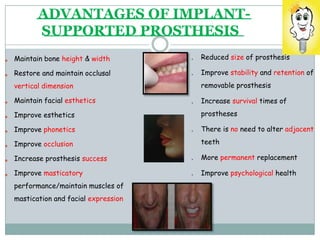
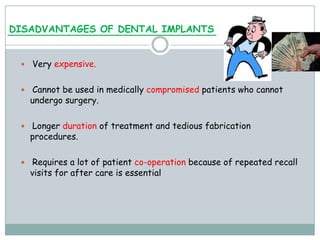
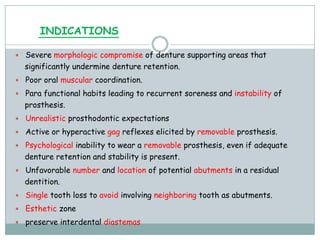
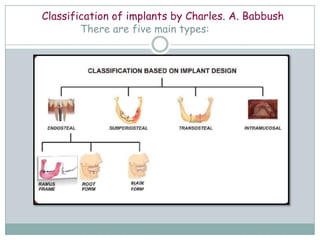
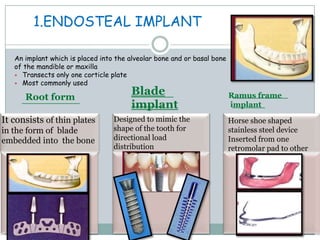
Dental implants are prosthetic devices surgically placed in the jaw to support crowns or dentures, offering significant advantages over traditional restoration methods. They enhance stability, retention, and aesthetics while preventing bone loss, but come with high costs and are not suitable for all patients. Various types of implants exist, each with distinct designs and materials suited for different clinical situations.

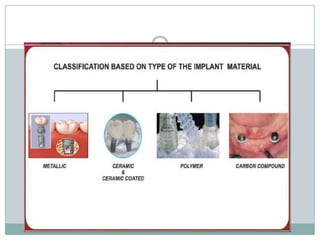
![• Depending on the materials used:
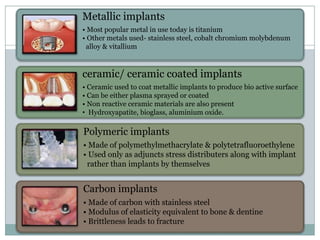
Metallic implants
[titanium, titanium alloy, cobalt chromium molybdenum alloy]
Non- metallic implants
[ceramics, carbon]
• According to loading
• Immediate(<2weeks)
• Early(2weeks -2mts)
• Delayed (>3mts)
• According to method of placement
• Tapping system
• Threading system](https://image.slidesharecdn.com/implants013948-220803081826-092f18da/85/Implants_013948-ppt-24-320.jpg)