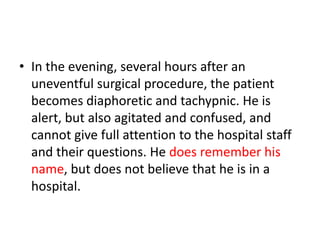
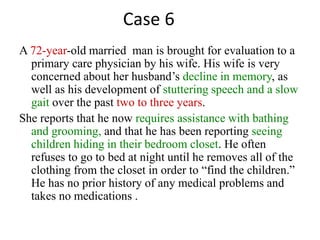
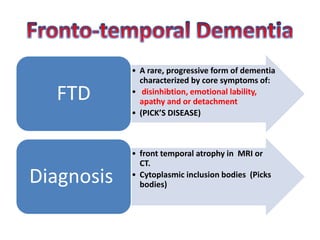
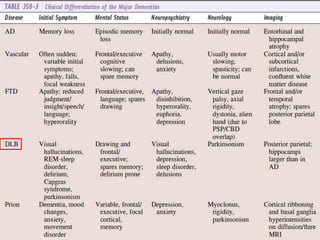
The document outlines various case studies related to different forms of dementia and cognitive disorders, detailing patient histories, symptoms, and diagnostic possibilities. It emphasizes the importance of medical history and assessment techniques in diagnosing conditions such as Alzheimer’s disease, vascular dementia, and Lewy body dementia, along with the role of cognitive examinations like the Mini-Mental State Exam. Additionally, it discusses the management and treatment options for these conditions, highlighting the variability in dementia presentations and the potential for reversible conditions.